On This Page:
Dissociation is a coping mechanism that some people use to deal with overwhelming or traumatic experiences. It involves a disconnection or detachment from one’s thoughts, emotions, sensations, or surroundings.
Dissociative experiences can range from mild (e.g., daydreaming) to severe (e.g., dissociative identity disorder). Some common symptoms of dissociation include feeling numb, spaced out, or disconnected from reality.
It’s important to seek professional help if dissociation is interfering with your daily life or causing distress.

What Does Dissociation Feel Like?
People who dissociate may feel detached from their bodies or feel as though the world around them is not real. Dissociation can happen for many people as a natural response to trauma that they cannot control.
Experiences of dissociation can last for a relatively short amount of time, as short as a few hours, or this feeling can last for much longer, as long as weeks or months.
Many people may experience dissociation during their lifetime, as it can be a way for the mind to cope with too much stress. If an individual dissociates for a long time, this may develop into a dissociative disorder.
Dissociation may become the main way someone copes with stressful experiences.
Dissociation can be detrimental as it can disrupt areas of functioning that usually work together automatically. These areas are consciousness, memory, identity, and awareness of the self and the environment.
People who experience dissociation may experience something called depersonalization. This is a feeling of being disconnected from the body, being outside of oneself, and observing your actions, thoughts, or feelings from a distance.
Also, people who disassociate may experience derealisation. This is where the world around the individual does not feel real, as if living in a movie.
The surroundings may appear distorted, two-dimensional, or artificial because of derealisation. Therefore, dissociation can range anywhere from a mild sense of detachment to a more severe disconnection from reality.
Personal Experience
Below are some quotes taken from individuals who have experienced dissociation.
“If a switch is oncoming, my vision starts to tremble (best word for it) and everything around me feels peculiarly distant and completely unreal, and the lights go extremely bright. The lights going funny is usually the first sign for me, then comes the trembling vision, then the faded reality. I can often “pull myself back” from that, but if it goes any further, there’s no chance.”
‘Bryan’
“you just don’t really feel like you’re here … time kind of elapses”
Participant from Černis et al. (2020).
“You try and get control of it, but it’s like a bar of soap or something, it just keeps slipping out of your hands.”
Participant from Černis et al. (2020).
“I wanted time to pass, but it didn’t, it seemed . . . It seemed I had already been there for 24 hours, at the moment, there.”
Participant from Mattos et al. (2016).
“I don’t feel present sometimes, thoughts are not here.”
Participant from Gušić et al. (2018).
“It is similar to a daydream, but you are even more removed than that. Sometimes I am at work and I am looking at what I’m doing, and I can hear everything around me just fine, but it feels like my peripheral vision is fuzzy, my energy is low, my mind is focused on something very far away.”
‘Leo’
Types of Dissociation
Dissociative identity disorder
Dissociative identity disorder (DID), renamed from multiple personality disorder in 1994, is a disorder that is categorized by the presence of two or more identities or personalities that an individual has.
These identities recurrently take control of the individual’s behavior, as well as resulting in them forgetting important personal information.
Dr Dawn-Elise Snipes, a Licenced Counselor, outlines some of the key alterations in functioning that occur when someone switches between alters/identities:
“The individual has two or more distinct personality states observed by others or experienced by the individual characterized by alterations in sense of self, affect, behavior, memory, perception, cognition and or sensory motor functioning may also change.”
An individual with DID may ‘switch’ to the alternating identities and may feel the presence of two or more people talking inside their head.
The other personalities may have their own names, personal histories, characteristics, style of voice, and mannerisms.
Dr Snipes goes on to explain what else can change during a switch:
“Attitudes, outlooks and personal preferences including food, activities.. (According to the DSM criteria) a person’s gender identity may change when they are in an alter they can have what they define as male alters they can have what they define as female alters.”
Depersonalization-derealisation disorder
This type of dissociative disorder is associated with the presence of persistent or recurrent experiences of depersonalization, derealization, or both.
People with this disorder may feel like a stranger to themselves and/or to their surroundings (their surroundings may feel unreal).
Psychiatrist Dr Tracey Marks explains that there is a sense of detachment from oneself and not recognizing your own reflection for instance:
“Some examples of this are looking in a mirror and not recognizing yourself, or seeing yourself as an observer in the room.”
Individuals with this disorder may also have a distorted sense of time, altered bodily perceptions, and numb emotions and bodily senses.
People with this disorder may also feel detached from the reality of their environment:
“You can also feel like you’re looking at things through a glass or you have tunnel vision. You can also feel like the things that you’re looking at are distorted. I had someone tell me that it’s like the world is tilted like this.”
Dr Tracey Marks, Psychiatrist
Dissociative amnesia
Dissociative amnesia is thought to be the most common dissociative disorder, with different types of amnesia branching from this condition. The main symptom of this disorder is memory loss which is more severe than typical forgetfulness.
One type of dissociative amnesia is localized amnesia, which is the failure to recall events of a specific period of time. Selective amnesia is when some, but not all, events can be recalled during a period of time.
Generalized amnesia, which is the rarest type, is when an individual’s life history is completely forgotten, and they may forget their identity.
Other specified dissociative disorders
This category includes dissociative disorders that do not meet the full criteria for any specific dissociative disorder but still cause significant distress or impairment in functioning.
Examples of other specified dissociative disorders may include atypical dissociative disorder, which involves dissociative symptoms that do not fit the criteria for any specific dissociative disorder but still cause significant distress or impairment, or acute dissociative reactions, which are temporary episodes of dissociation that occur in response to a stressful or traumatic event.
Unspecified dissociative disorder
Unspecified dissociative disorder is applied to people whose symptoms are characteristic of a dissociative disorder but do not meet the full criteria for any of the specific disorders mentioned above.
This unspecified category is often used in situations where a doctor or clinician chooses not to specify which, if any, disorder an individual may have due to there being insufficient information to make an actual diagnosis.
Signs of Dissociative Disorders
Symptoms associated with dissociative disorders vary depending on the type of disorder being experienced. Please note that dissociation can manifest in different ways and with varying degrees of severity.
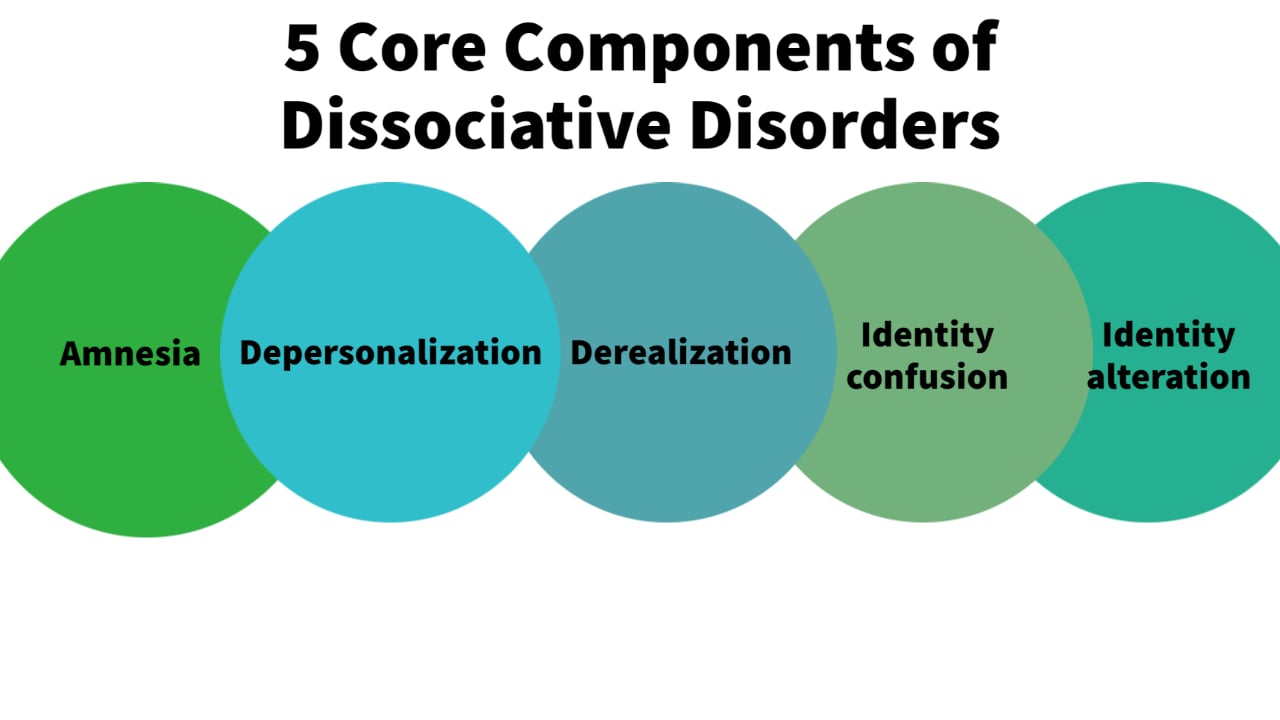
It is understood there are five core components of dissociative disorders. Each dissociative disorder could be described and understood using a combination of one of these five core symptoms:
-
Amnesia – memory loss of certain time periods, events, people, and personal information, which are recurrent.
These gaps in memory can vary from several minutes to years and are inconsistent with typical forgetting.
-
Depersonalization – a sense of detachment or disconnection from oneself and their emotions. This can include feeling like a stranger to oneself, being on autopilot, or feeling like a part of their body does not belong to them.
Often, individuals who experience depersonalization may induce injuries to themselves in order to feel ‘real.’
-
Derealization – the perception of the familiar people and surroundings around an individual as being distorted and unreal. For instance, close friends or relatives may not seem real to an individual experiencing derealization.
The world around them may also appear distorted or blurred or artificial in general. Some episodes of derealization may happen during flashbacks, whereby an individual may feel much younger than they are and feel as if the present environment is unreal at that time.
-
Identity confusion – some people with dissociative disorders may have a blurred sense of their own identity. This may involve an inner struggle regarding an individual’s sense of self or identity, with feelings of conflict and uncertainty.
-
Identity alteration – this is a sense of acting like a different person some of the time and in different situations.
Individuals who experienced this may use different names depending on the situation, realize they have items that they do not recognize, or may have learned a new skill that they have no recollection of learning.
Usually, if any of the core components of dissociation are being experienced, that are persistent, cause significant distress, disrupt important areas of functioning, and cannot be explained by other means (e.g., through alcohol or mind-altering drugs), this could be an indication that an individual may be experiencing a dissociative disorder.
Although, keep in mind that only a professional should diagnose a dissociative disorder, and advice should be sought if someone believes they may be experiencing the above signs.
Why Do I Dissociate?
Dissociation is a psychological experience that can occur in response to various factors, including trauma, stress, or other types of overwhelming experiences. Below are some potential causes of dissociation.
Note that these causes may only contribute to fleeting dissociative feelings. If the symptoms of dissociation persist and they meet the diagnostic criteria, this could result in a dissociative disorder.
Trauma
Trauma is a significant cause of dissociation, especially severe trauma during childhood. For example, ongoing physical, sexual, or emotional abuse from a parent or other caregiver can overwhelm a young child’s ability to cope and cause them to dissociate.
Other potential childhood traumas that may trigger dissociation include witnessing domestic violence between parents, the death of a close family member, injuries and medical procedures, or surviving a natural disaster.
Particularly, if trauma has been experienced before the age of 5, this makes it more likely that the child will dissociate as a coping mechanism. For an adult, trauma from combat, violent assaults, accidents, or natural disasters can also cause dissociation.
Essentially any event that overwhelms the person’s ability to cope may trigger a dissociative response.
Stress
High levels of emotional stress can also trigger dissociation in some people. Examples of severe life stressors that could overwhelm a person’s coping capacities include the loss of a loved one, divorce, job loss or instability, physical illness, bullying, or financial pressures.
When a person experiences stress, their body’s natural response is to activate the “fight or flight” response, which prepares the body to deal with a perceived threat.
However, if the stressor is ongoing or the person is unable to escape the stressor, the body may enter a state of freeze or shutdown (dissociation).
The key aspect is that the stressor persists and the individual feels trapped or unable to escape the distress.
For instance, a person under intense work stress who feels overwhelmed and powerless may begin to feel detached from themselves, causing dissociation. Or someone going through a difficult breakup may disconnect from the pain of loss through derealization.
In both cases, dissociation serves as an emergency coping response when normal coping mechanisms fail.
Substance use
Another known cause for dissociative disorders may be substance use. The use of some recreational drugs, such as ecstasy and Ketamine, can cause some feelings of dissociation whilst taking them.
This dissociation would only be considered a disorder if the signs of dissociation continued after stopping using the drugs.
Anxiety and depression
Anxiety and depression may cause dissociation as a way to cope with overwhelming emotions or thoughts.
For anxiety, the associated fear and worry can become so intense that the person may dissociate to protect themselves from the emotional pain.
Similarly, depression can also lead to dissociation as a way to cope with overwhelming feelings of sadness or hopelessness.
In both cases, dissociation can provide a temporary escape from the intensity of the emotions or thoughts associated with anxiety or depression.
Sleep deprivation
Sleep deprivation can cause dissociation as a result of the brain’s inability to process information and regulate emotions and behavior effectively.
During sleep, the brain undergoes critical processes for consolidating memories, processing emotions, and restoring energy levels. When a person is sleep-deprived, these processes are disrupted, leading to a range of cognitive and emotional impairments, which may trigger dissociation.
A sleep-deprived person may experience difficulties with focusing, making decisions, or processing sensory information. They may also have trouble distinguishing between reality and imagination or experience depersonalization.
Complications of Dissociative Disorders
If left untreated, symptoms of dissociation can become lifelong and detrimental across multiple areas of functioning (Hoyos et al., 2019).
Dissociation greatly increases one’s vulnerability to self-harm and suicidal behaviors, with over 70% of people with dissociative disorders reporting past suicide attempts (Foote et al., 2008).
Chronic dissociation is also associated with difficulty maintaining employment and relationships, as well as an increased risk of substance abuse as a maladaptive coping mechanism (Batey et al., 2010).
The combination of dissociation and PTSD specifically puts adolescents at 3.5 times greater likelihood of engaging in sexual risk-taking behaviors (Kisiel & Lyons, 2001).
Letting dissociative symptoms persist may also lead to worsening the severity of other mental illnesses over time (Tull, 2022).
Given the risk of self-harm, revictimization, job loss, relationship problems, worsening mental health, and other issues, it is critical to seek professional treatment for ongoing dissociation.
Evidence-based interventions like trauma-focused therapy and grounding techniques can help reduce dissociative symptoms and improve functioning across major life areas (Hoyos et al., 2019).
How Can Dissociative Disorders be Managed?
The treatment for dissociation depends on the underlying cause and severity of the symptoms.
Self-care
For individuals who experience mild dissociative symptoms, self-care techniques can help to manage dissociative symptoms:
- Grounding exercises – Activities like mindful breathing, progressive muscle relaxation, or tapping exercises can help reconnect you to the present moment.
- Prioritizing sleep – Getting adequate, high-quality sleep helps the brain properly consolidate memories and process emotions disrupted by dissociation.
- Creative expression – Art therapy, journaling, or music therapy gives an outlet to process traumatic memories that may be triggering dissociation.
- Stress reduction – Lowering your stress levels through healthy diet, exercise, social support, or relaxation practices can help minimize dissociation triggers.
- Reality checking – Using reminder notes or safety objects keeps you oriented to the here-and-now and combats feelings of unreality from derealization.
Practicing regular self-care builds critical coping skills for interrupting dissociation and staying grounded in your body and surroundings. Over time, this can help reduce dissociative symptoms.
Psychotherapy
For individuals with more severe dissociative symptoms or a dissociative disorder, professional treatment such as psychotherapy may be necessary.
Psychotherapies are a collection of talking therapies that usually involve discussing the symptoms and techniques to help cope, working with the other identities (for DID), and helping the individual to understand their condition, including what may be the underlying cause.
Cognitive behavioral therapy (CBT) is a type of psychotherapy that helps people identify and modify thought patterns that may be disturbing and negatively influence behavior and emotions.
CBT involves working together with the therapist to practice new thinking skills, set goals, and problem-solve. It also involves completing CBT tasks between therapy sessions, so these skills are thoroughly practiced, becoming a habit.
CBT has shown effectiveness for many people, with a study reporting that those who completed CBT had significant reductions in their levels of dissociation and depersonalization, with 29% no longer meeting the criteria for dissociative disorders after treatment (Hunter et al., 2005).
Dialectical behavior therapy (DBT) is another type of CBT. Its main goal is to help individuals develop healthy ways to cope with stress, regulate their emotions, and improve relationships with others. DBT has a big focus on mindfulness skills.
Eye Movement Desensitization and Reprocessing (EMDR) is a type of therapy that can be effective in treating trauma-related dissociation. It involves guided eye movements that help the individual process traumatic memories and reduces the associated distress.
Likewise, creative therapies such as art therapy, music therapy, and other creative therapies can be helpful in treating dissociation by providing an outlet for self-expression and a way to process traumatic experiences.
Medication
Currently, there are no medications that are specifically targeted to treat dissociative disorders themselves. However, people with these conditions may take medication for some symptoms or other conditions they may have alongside dissociation.
For instance, if someone is experiencing dissociation, they may also have a depressive or anxiety disorder. Some medications, such as antidepressants, can be used for depressive and anxious symptoms. Similarly, benzodiazepines, a type of sedative medication, can also be used for anxiety.
Overall, the treatment for dissociation is typically a combination of therapy, medication, and self-care techniques. It’s important to work with a mental health professional to develop an individualized treatment plan that addresses the specific needs of each person.
Do you need mental health help?
USA
Contact the National Suicide Prevention Lifeline for support and assistance from a trained counselor. If you or a loved one are in immediate danger: https://suicidepreventionlifeline.org/
1-800-273-8255
UK
Contact the Samaritans for support and assistance from a trained counselor: https://www.samaritans.org/; email jo@samaritans.org.
Available 24 hours a day, 365 days a year (this number is FREE to call):
116-123
Rethink Mental Illness: rethink.org
0300 5000 927
References
Batey, H., May, J., & Andrade, J. (2010). Negative intrusive thoughts and dissociation as risk factors for self-harm. Suicide and Life-Threatening Behavior, 40(1), 35–49.
Černis, E., Freeman, D., & Ehlers, A. (2020). Describing the indescribable: A qualitative study of dissociative experiences in psychosis. PLoS One, 15(2), e0229091.
Dissociative Identity Disorder. (Jul 05, 2021). Traumadissociation.com, Retrieved Jul 5, 2021, from http://traumadissociation.com/dissociativeidentitydisorder.html.
Traumadissociation.com. Retrieved Jul 5
Dissociative Amnesia & Fugue. (Jul 05, 2021). Traumadissociation.com, Retrieved Jul 5, 2021, from http://traumadissociation.com/dissociativeamnesia.html.
Depersonalization/Derealization Disorder. (Jul 05, 2021). Traumadissociation.com. Retrieved Jul 5, 2021 from http://traumadissociation.com/depersonalization.html.
Foote, B., Smolin, Y., Neft, D. I., & Lipschitz, D. (2008). Dissociative disorders and suicidality in psychiatric outpatients. The Journal of Nervous and Mental Disease, 196(1), 29–36.
Gušić, S., Malešević, A., Cardeña, E., Bengtsson, H., & Søndergaard, H. P. (2018). “I feel like I do not exist:” A study of dissociative experiences among war-traumatized refugee youth. Psychological Trauma: Theory, Research, Practice, and Policy, 10(5), 542.
Hoyos, C., Mancini, V., Furlong, Y., Medford, N., Critchley, H., & Chen, W. (2019). The role of dissociation and abuse among adolescents who self-harm. Australian & New Zealand Journal of Psychiatry, 53(10), 989–999.
Hunter, E. C., Baker, D., Phillips, M. L., Sierra, M., & David, A. S. (2005). Cognitive-behaviour therapy for depersonalisation disorder: an open study. Behaviour research and therapy, 43(9), 1121-1130.
Kisiel, C. L., & Lyons, J. S. (2001). Dissociation as a mediator of psychopathology among sexually abused children and adolescents. American Journal of Psychiatry, 158(7), 1034–1039.
Mattos, P. F., Pedrini, J. A., Fiks, J. P., & de Mello, M. F. (2016). The concept of peritraumatic dissociation: A qualitative approach. Qualitative Health Research, 26(7), 1005-1014.
Steinberg, M., Rounsaville, B., & Cicchetti, D. V. (1990). The Structured Clinical Interview for DSM-III—R dissociative disorders: Preliminary report on a new diagnostic instrument. The American Journal of Psychiatry.

