On This Page:
- Depersonalization is a dissociative disorder that affects a person’s perception of themselves and their surroundings. It is characterized by recurring episodes of depersonalization, derealization, or both.
- Depersonalization involves feeling detached from oneself, as if observing one’s thoughts, emotions, and actions from a distance. Derealization, on the other hand, involves feeling that the world around is unreal, distorted, or dreamlike. People and objects may appear fuzzy, lifeless, or two-dimensional.
- Other symptoms include feeling emotionally numb, disconnected from one’s surroundings, and experiencing memory difficulties.
- If you suspect you may be experiencing depersonalization/derealization disorder, it is important to seek the help of a mental health professional.

What is depersonalization?
Depersonalization is a complex symptom that can be defined as ‘a state in which the sense of self and the quality of subjective first-person experience are oddly altered’ (Medford, 2012).
It can be described as feeling disconnected from the self or feeling as though you aren’t real.
It can be normal to feel depersonalization from time to time, especially in times of stress, upset, fatigue, or with drug use. Transient episodes of depersonalization have a lifetime prevalence between 26% and 74% of someone experiencing at least one episode.
What is derealization?
Derealization is also a part of the disorder, and this symptom affects how individuals relate to other people and their environment. They may feel as if their surroundings or other people are not real.
While depersonalization is defined as disconnections from the self, derealization is defined as disconnections from external reality.
Derealization is conceptualized as a sense of “unreality or detachment from, or unfamiliarity with, the world, be it individuals, inanimate objects, or all surroundings” (APA, 2013, p. 303).
A person who experiences derealization might feel as though they are in a fog or a dream or that the surrounding world is somehow artificial and unreal.
When does depersonalization become a disorder?
For most people who depersonalize, this feeling will usually diffuse once the stressful situation is over or once the drug has run its course (if caused by drug use).
Often, depersonalization is viewed as the mind’s defense mechanism to help cope with stressful situations.
Feelings of depersonalization can become pathological when the individual is unable to control when and where these symptoms occur, when the depersonalization becomes generalized to other situations and circumstances, or when it persists beyond the presence of a stressor.
In this situation, it is possible that the individual may have what was previously known as depersonalization disorder, now known as depersonalization/derealization disorder (DPDR).
DPDR is classified as one of 3 dissociative disorders, the others being dissociative amnesia and dissociative identity disorder.
Dissociative disorders are mental conditions involving disruptions or breakdowns in awareness, consciousness, and memory. For people with DPDR, the periods of dissociation can last for a relatively short amount of time (minutes or hours), or sometimes much longer (days, weeks, months, or years).
Most people with DPDR develop it when they are young. The average age for the onset of DPDR is 16, with the condition rarely beginning after the age of 40. The prevalence of this disorder is thought to affect around 1-2% of the general population (Hunter et al., 2004).
Symptoms
Individuals who experience depersonalization might believe their thoughts and feelings are not their own.
They may feel robotic, as though they lack control over their movements and speech; they may experience a distorted sense of time, and, in extreme cases, they may sense an “out-of-body” experience in which they see themselves from the perspective of another person.
Individuals with DPDR often have difficulty describing their symptoms and may think they are ‘going crazy’ (APA, 2013).
It is worth noting that DPDR can present differently in everyone. The specific traits and difficulties that individuals with DPDR experience can be unique and may vary in severity. Not everyone with DPDR will experience all of the symptoms.
Likewise, many people may identify with one or more symptoms of the disorder but may not qualify for a full diagnosis.
Below are some of the key symptoms of DPDR:
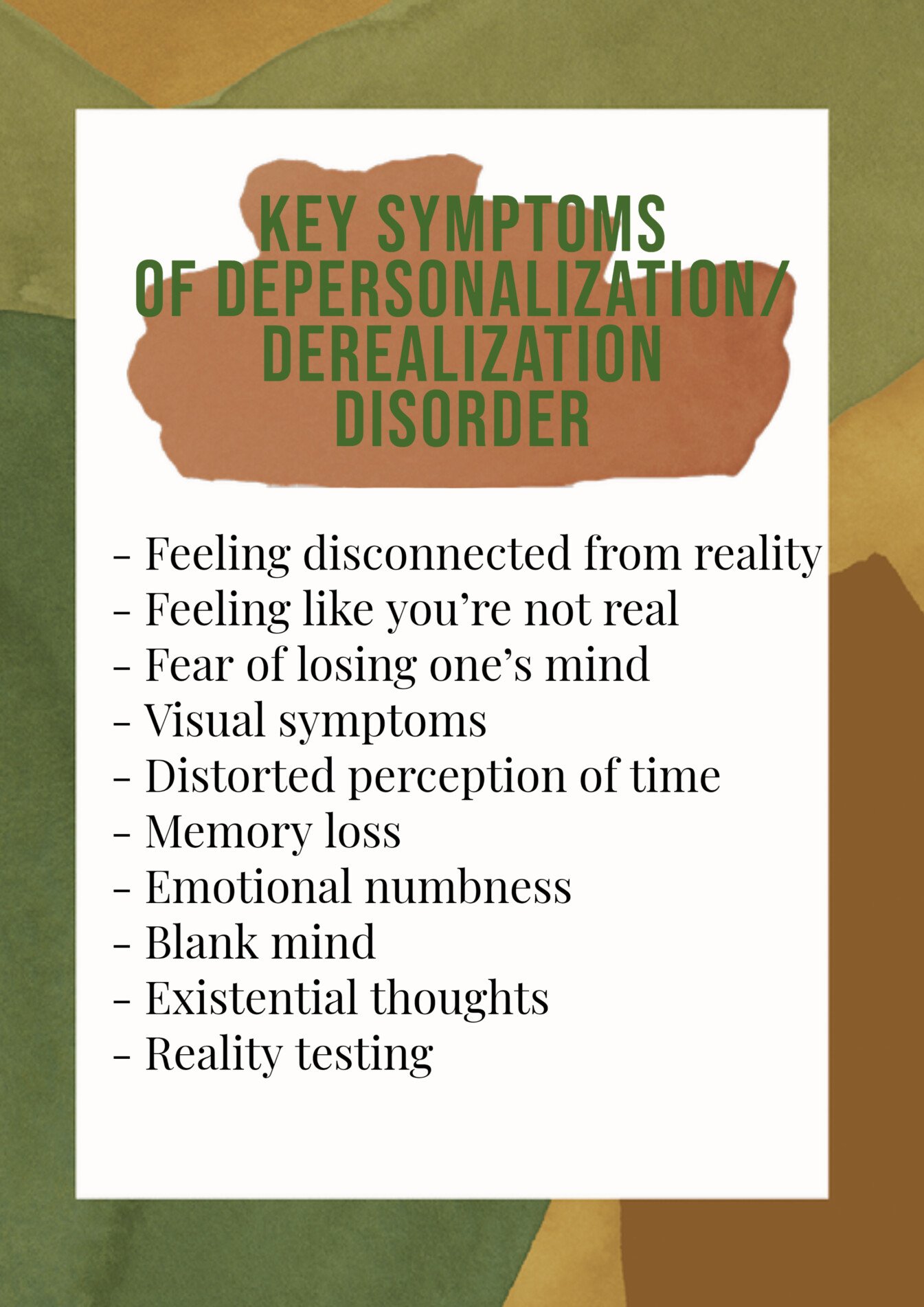
Feeling disconnected from reality
People who experience depersonalization may feel as if there is a barrier between themselves and the world. They may feel as though they are living in a dream or that things around them are not real.
Feeling like you’re not real
People may feel their movements and actions do not feel like their own. They may feel as though they are watching someone else. Sometimes people will report feeling as if they are watching themselves from the outside, as if they are an onlooker.
Fear of losing one’s mind
Many people may worry that their depersonalization symptoms will become so intense that they could be insane. However, depersonalization is the brain reacting to what it perceives as danger, although it is not always accurate.
Visual symptoms
Many people who experience depersonalization report visual symptoms such as tunnel vision, distorted and blurry vision, experiencing floaters in their vision, or the distance and size of objects being altered.
A possible explanation is that when anxious, the eyes naturally become more sensitive to picking up movements by dilating the pupils to let more light in.
This can make it feel as if there is too much visual information coming in at once.
Distorted perception of time
Often, people may report that they feel like time goes by too fast, there are gaps of time that are forgotten, they find they jump from one moment to another, recent events feel old, or old events feel recent.
This may be happening because the anxiety is affecting the concentration of individuals, so the passing of time feels different. The racing thoughts that they have could distract them from the time going by.
Memory loss
Occasionally, those experiencing depersonalization may have issues with their memory. They may forget what they were doing or saying, cannot remember what happened the day previously, or feel as if they are losing their short or long-term memory.
However, this is likely the anxiety affecting memory, as anxiety usually affects concentration. This can make it seem like the memories have gone blank, and one cannot focus on the task at hand.
Emotional numbness
This symptom is described as an inability to feel happy, sad, or any emotion. An explanation for why this may happen is that since depersonalization is a defense mechanism that keeps someone safe, it can make them feel distant and cut off.
Pairing this with racing thoughts and finding it difficult to concentrate can make things feel worse.
There is nothing wrong with the person’s emotions or the ability to feel them; these are only the temporary effects of anxiety and its symptoms.
Blank mind
People who depersonalize often find that their mind is empty, their thoughts are gone, or they cannot put a thought together. Having a blank mind is often described as losing one’s inner monologue.
However, you only experience this inner monologue when not consciously thinking about it, so if individuals are constantly trying to see if this is present, they are often interrupting it.
Existential thoughts
As depersonalization is a bizarre experience, the rational brain is desperately trying to find an explanation as to what is causing this.
Often, people may attribute the bizarre feelings to having significance, such as thinking they may be in a coma, dreaming, or purgatory, for instance.
Our brains tend to want big explanations, so it often jumps to the scariest conclusions – this is known as catastrophizing.
Reality testing
Those affected by depersonalization may believe they are experiencing psychosis due to some of the symptoms mentioned earlier. However, the big distinction with depersonalization disorder is that the individuals have intact reality testing.
This is the objective evaluation of an emotion or thought against real life. So even with the most frightening thoughts, one can always distinguish between thoughts and reality.
Some people with DPDR may experience mild, short-lived symptoms, while others have chronic symptoms that may last for years.
The symptoms may be very distressing to the point where they interfere with their ability to function in daily life, including at work, school, or in relationships.
Are symptoms similar to other disorders?
The symptoms of depersonalization may be observed in other disorders, such as anxiety disorders such as post-traumatic stress disorder (PTSD), and panic disorder, as well as depression and schizophrenia.
Those with DPDR frequently experience cognitive symptoms of increased arousal paired with subjective deficits in attention and concentration, as seen in anxiety disorders. High levels of co-existing anxiety have been found in people with DPDR (Michal et al., 2016).
Causes and risk factors
There is not always a clear cause for what causes depersonalization and DPDR. In a lot of cases, care providers are not able to identify what triggers this disorder in patients.
Many people with this disorder report a history of childhood trauma, particularly emotional abuse and neglect. For someone growing up in a household with a lot of violence or yelling, they may have mentally removed themselves from those situations as a coping mechanism.
Thus, as adults, they may fall back onto these dissociating tendencies in stressful situations. Or they may find that they dissociate when there is no known trigger, but it could link back to their childhood trauma.
Some people may find that they depersonalize after experiencing trauma or intense stress which did not occur in childhood. This may occur after the following:
-
Witnessing or experiencing abuse
-
An accident
-
Encountering a life-threatening danger
-
Natural disasters
-
The death of a loved one
-
Violence or war
Hunter et al. (2003) proposed that depersonalization disorder is most often triggered by one’s response to situations that provoke anxiety. This symptom overlap and high comorbidity of DPDR with anxiety disorders indicate there may be a link between DPDR and anxiety.
Some other causes of depersonalization include:
-
Certain drugs, such as hallucinogens
-
Extreme fatigue and sleep deprivation
-
Physical conditions such as seizure disorder
-
Living with a parent who has a severe mental illness
-
A co-existing mental health condition
Treatment options
In terms of treatment, this depends on the severity of the depersonalization symptoms being experienced and whether DPDR is diagnosed.
During periods of acute stress or some episodes of depersonalization, supportive interventions such as coping skills and strategies may be a good fit.
Whereas, during periods of mild to more severe symptoms and a diagnosis of DPDR, other approaches may be required.
Medication
There are currently no known medicative treatments for DPDR. While there is no specific medication, antidepressants may be helpful, especially if there is underlying depression or anxiety alongside DPDR.
However, for some people, antidepressants may actually increase depersonalization or derealization symptoms. Trials of a type of antidepressant called selective serotonin reuptake inhibitors (SSRIs) with people who had a diagnosis of DPDR found that this medication may induce some of the symptoms to make the condition worse (Brand et al., 2012).
Otherwise, atypical antipsychotic medications that block both dopamine and serotonin receptors may be useful in treating some cases of DPDR with ‘psychotic features.’
It is worth noting that medications can come with possible side effects and may not be suitable for everyone. It is advisable to speak to a professional if you are considering meditative treatment.
Psychotherapies
Psychotherapies such as psychodynamic or cognitive behavioral therapy (CBT) may be effective for managing the symptoms of DPDR.
Psychodynamic psychotherapy uses self-reflection and self-evaluation achieved through cooperation and interrelationship with a psychiatrist. The expectation is that the patient will explore effective coping strategies and relationship patterns.
The psychiatrist will attempt to reveal the unconscious components of the patient’s maladaptive functioning to tackle the symptoms being experienced.
CBT is focused on identifying and adjusting unhelpful thinking patterns, feelings, and behaviors with a therapist.
Through working with the therapist, the patient can find ways to switch to more realistic thinking patterns and learn coping techniques that can be practiced in times of stress.
Hunter et al. (2005) published a study of patients who received an average of 13 CBT sessions. They found that patients had reductions in their levels of dissociation and depersonalization, with 29% no longer meeting the diagnostic criteria of DPDR after treatment.
Aside from psychodynamic therapy and CBT, people may opt for one of the following:
-
Dialectical behavior therapy (DBT) – this is a type of CBT that may help individuals with tolerating difficult emotions, including dissociative symptoms. It may also be useful for those who have experienced abuse or trauma.
-
Family therapy – working together, the individual’s family can learn about depersonalization. The group can learn how to recognize signs of when this occurs and offer their support when it does.
-
Creative therapies – art or music therapy can help individuals to explore and express their thoughts and feelings in a safe and creative environment.
Managing DPDR
When experiencing episodes of depersonalization, some techniques can be used to help make the symptoms more manageable.
-
Acknowledge your feelings
Often, acknowledging what you are feeling and the emotions being experienced can help to lessen these feelings.
It may be helpful to name the emotion you are experiencing to bring awareness and understanding to your feelings.
-
Breathing exercises
When moments of stress and anxiety arises, the body’s sympathetic nervous system fires up, which can lead to feelings of depersonalization.
Breathing exercises, especially deep breathing, may help reset the nervous system, calming it down. Guided meditation and mindfulness training usually include deep breathing and can also calm the body down.
-
Listen to music
Feelings of depersonalization can become more intense when the brain focuses on them. Using a grounding technique, such as listening to music, may help you feel less anxious about the experience.
Music has been known to reduce cortisol levels, a stress hormone. It may be useful to keep a specific playlist of favorite songs which can be played when experiencing depersonalization symptoms.
-
Read a book
Reading a book may be another way to help with the anxious thoughts that often occur alongside depersonalization. This may help to focus the mind on something else, interrupting the intrusive thoughts.
Concentrating on the words and being immersed in a story could help ease negative thoughts.
-
Challenge intrusive thoughts
Some people who experience depersonalization may have a lack of intrusive thoughts. However, for others, especially if they also have anxiety disorders or PTSD, intrusive thoughts can pose a challenge.
There is a tool called psychological distancing which can be used to help quiet intrusive thoughts.
Psychological distancing means one finds space between upsetting thoughts and painful emotions. You may ask yourself what evidence there is that the intrusive thoughts are real.
Finding that there is little to no evidence that these thoughts are real can help provide realistic and rational thoughts over intrusive thoughts.
-
Talk to a trusted friend
Often when experiencing depersonalization, it is tempting to isolate yourself away from others. But at these times, talking to a trusted friend or family member may help.
Sharing these struggles with others can help you feel better. As well as this, others may provide some useful advice or insight which can further help you.
-
Getting enough sleep
Although this is more of a longer-term method, going to sleep when the body feels tired can help with managing stress and decrease anxiety.
Some people may experience depersonalization due to being fatigued, so keeping a regular sleeping schedule can be really beneficial to mental health.
Also, keeping bedtime as relaxing as possible can aid in better sleep, such as ensuring that phones or other screens are not used in bed or before trying to sleep.
-
Exercise
Engaging in exercise is often proven to help with managing stress and can be beneficial to mental health. Aerobic exercise, for instance, could help decrease burnout as a result of depersonalization.
-
Engaging your senses
If you find yourself in a situation where you feel the symptoms of depersonalization starting to creep up on you, it can be useful to try engaging all your senses.
Being able to engage the senses can help with checking that you are real and can also help in grounding yourself in your body and surroundings.
Engaging the senses can include holding ice cubes, eating sour candy, smelling spices, strong coffee, or essential oils.
Related Articles
References
American Psychiatric Association, D. S., & American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (Vol. 5). Washington, DC: American psychiatric association.
Brand, B. L., Lanius, R., Vermetten, E., Loewenstein, R. J., & Spiegel, D. (2012). Where are we going? An update on assessment, treatment, and neurobiological research in dissociative disorders as we move toward the DSM-5. Journal of Trauma & Dissociation, 13(1), 9-31.
Hunter, E. C. M., Phillips, M. L., Chalder, T., Sierra, M., & David, A. S. (2003). Depersonalisation disorder: a cognitive–behavioural conceptualisation. Behaviour Research and Therapy, 41(12), 1451-1467.
Hunter, E. C., Baker, D., Phillips, M. L., Sierra, M., & David, A. S. (2005). Cognitive-behaviour therapy for depersonalisation disorder: an open study. Behaviour research and therapy, 43(9), 1121-1130.
Hunter, E. C., Sierra, M., & David, A. S. (2004). The epidemiology of depersonalisation and derealisation. Social psychiatry and psychiatric epidemiology, 39(1), 9-18.
Medford, N. (2012). Emotion and the unreal self: depersonalization disorder and de-affectualization. Emotion Review, 4(2), 139-144.
Michal, M., Adler, J., Wiltink, J., Reiner, I., Tschan, R., Wölfling, K., Weimert, S., Tuin, I., Subic-Wrana, C., Beutel, M. E. & Zwerenz, R. (2016). A case series of 223 patients with depersonalization-derealization syndrome. BMC psychiatry, 16(1), 1-11.

