From time to time, everyone experiences sadness. People who are sad may find relief in crying, talking about their problems, or perhaps cheering themselves up using humor.
If the sadness does not pass or if the person is finding it difficult to resume their normal functioning, this could be a sign of depressive signs.
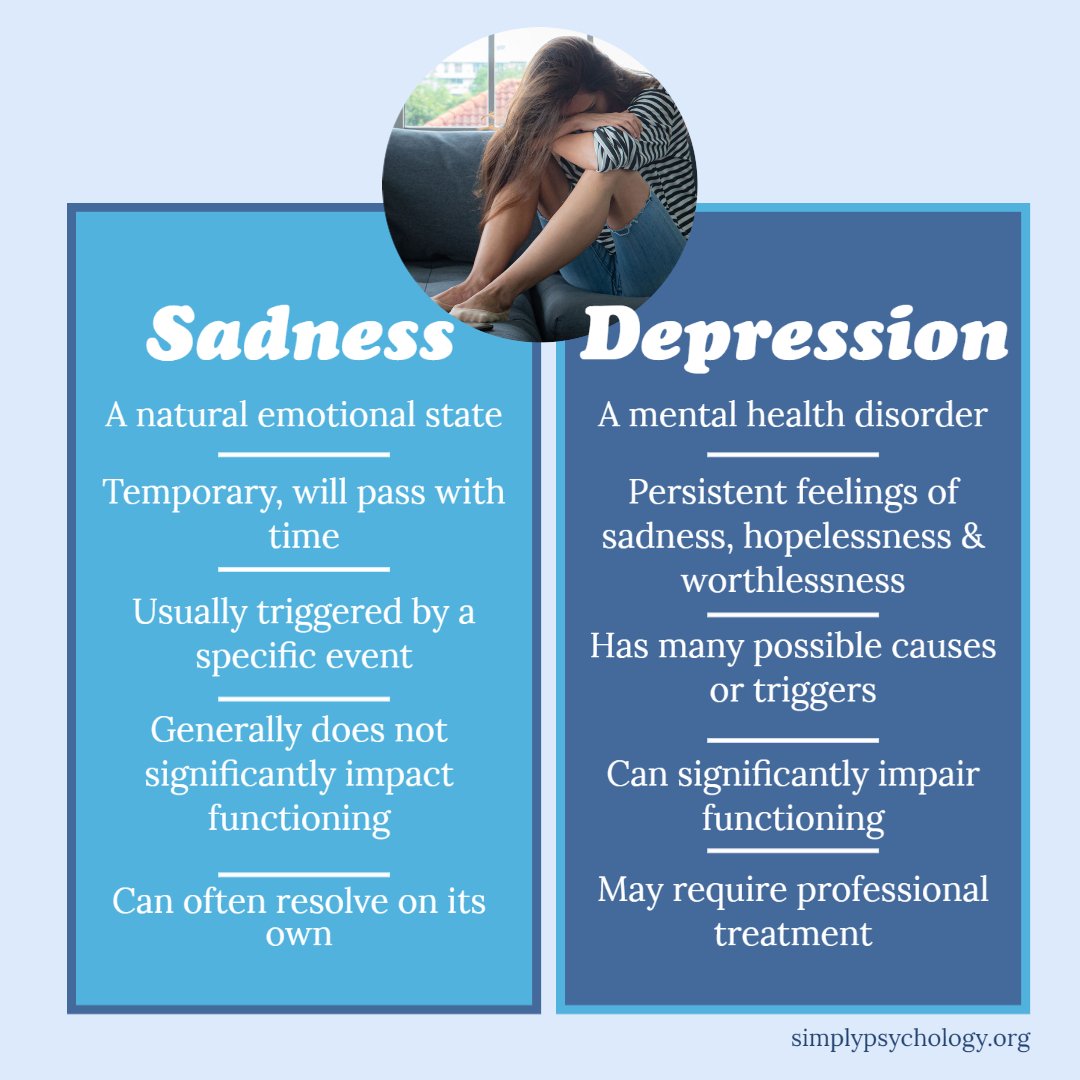
Sadness and depression are two distinct emotional states. Sadness is a natural human emotion that is typically triggered by a specific event, such as the loss of a loved one or a disappointment. It is usually a temporary feeling that can be resolved with time and support.
On the other hand, clinical depression is a longer-term mental health condition where a person often feels depressed mood most days, impairing social, occupational, and other important areas of normal functioning.
How do I know if I’m Depressed or just sad
According to Alex Korb, Ph.D., author of The Upward Spiral:
“Depression is not just sadness. It’s a complex set of emotions and physical changes that include not being able to get out of bed, not feeling motivated to do the things you love, feeling hopeless and helpless.”
When feeling sadness, it may feel all-encompassing at times, but there should be moments when people can feel comforted or able to experience happiness in most other aspects of their lives.
Those with depression, however, find that their depressed feelings will affect all aspects of their lives and may find it hard or even impossible to find enjoyment in anything, including activities they used to enjoy.
Depression is more than an emotion; it is a mental illness.
Those with clinical depression may not just experience sadness; they can also have intense feelings of helplessness, hopelessness, and feeling worthless. They may describe an ‘empty’ feeling inside and believe life is not worth living.
In sadness, a person may feel regret or remorse for something, but they will not experience any permanent sense of worthlessness or guilt as in depression. A person who is sad may cry, spend some time alone, then return to normal within a short span of time.
This is not the case for someone with depression, who often finds their feelings last for weeks or months.
Clinical depression is a common worldwide illness, with an estimated 3.8% of the population being affected (World Health Organization).
Depression can present differently to everyone. For some, their depressive episodes can result in suicidal ideation, self-harming behaviors, or suicidal attempts. Others may not present with these signs but still find day-to-day life difficult due to their depression signs.
“One of the most important things to remember about depression is that it’s not your fault. It’s not something you brought on yourself, it’s not a character flaw, and it’s not a sign of a weak personality.”
Alex Korb, Ph.D
Am I Depressed? – Signs of depression
Below are some of the signs that could be experienced by someone with depression. Note that signs of depression present differently in everyone and in severity, and not everyone will experience every signs:
Physical Signs
- Change in appetite
- Bowel changes
- General appearance; looking sad and miserable or unkempt
- Sexual dysfunction
- Sleep disturbance
- Fatigue
- Other: indigestion, palpitations, headaches, tight band round chest and head feelings, skin-picking, hand-wringing, general aches, and pains.
Psychological Signs
- Feelings of sadness, feeling low, or flat
- Feeling fed up, indecisive, preoccupied with physical sensations, indifference
- Loss of interest and reduction of participation in daily life
- Slow and monotonous speech
- Negative talk
- Poor concentration
- Preoccupation with morbid thoughts
- Feelings of being a failure
Types of depression
Depression can take form in many different mood types depending on the cause and the signs being experienced:
- Major depressive disorder
- Seasonal Affective Disorder
- Disruptive mood dysregulation disorder
- Premenstrual dysphoric disorder
- Substance-induced mood disorder
- Persistent depressive disorder also called dysthymia
- Depressive disorder due to another medical condition
- Postnatal/perinatal depression
Depression may have other features alongside it, such as:
- Anxious distress – when anxiety is experienced alongside the depressed feelings
- Mixed features – both depression and mania is present.
- Atypical features – an individual can feel good after happy events but also feel hungrier, need to sleep a lot, and are sensitive to rejection
- Psychotic features – this is where hallucinations or delusions may be present
- Catatonia – an individual cannot move their body normally – either still and unresponsive or have uncontrollable movements
Why Am I Depressed? – Causes and risk factors
There is not always a known or direct cause for what triggers the onset of depression. It could be that a combination of a variety of factors causes depression, such as:
- Genetics – as like many other mental health disorders, mood disorders such as depression can tend to run in families
- Trauma – if negative events are experienced at an early age, this can cause long-term changes in how the brain responds to fear and stress.
- Life circumstances – including relationship changes, finances, and where someone lives.
- Other medical conditions – people with a history of sleep problems, medical illnesses, chronic pain, and anxiety are more likely to develop depression. Some medications could also cause some signs of depression.
Studies on the beliefs that people with depression have about the causes of the condition have identified various probable causes (Khalsa et al., 2011).
These include interpersonal problems (such as poor social skills and mistreatment by others), developmental events (such as childhood problems and unresolved family issues), personality or cognitive causes (such as irrational concerns, emotional upset, and depressive ways of thinking), biological factors (e.g., genetics and biochemical imbalances), and environmental factors (e.g., stress, illness of self and others).
Life events
A change in life events could be a potential cause of a rise in depression, such as financial worries or worries about health.
With the COVID-19 outbreak, more people have isolated themselves for a long time, sometimes separating themselves from their support networks, not being able to do the activities that they find enjoyment in, and worrying about the world and people’s health.
As a result, research may find that, consequently, more people are finding themselves depressed or suffering from other mental health issues.
Biological causes
A common biological theory of depression is an imbalance of neurotransmitters in the brain.
Neurotransmitters are chemical messengers that travel through the brain’s nerve cells (neurons). The neurons help to transmit the neurotransmitters to the next neurons by attaching to receptor sites on the postsynaptic neuron so that they can influence the brain, mood, and behavior.
There are three key neurotransmitters that are believed to play a role in depression:
- Serotonin – a key hormone that stabilizes mood, feelings of well-being, and happiness.
- Dopamine – plays a role in motivation, reinforcement, pleasure, and reward.
- Norepinephrine – plays a role in arousal, energy levels, attention, and the regulation of emotions.
This theory of depression explains that serotonin, dopamine, and norepinephrine levels are low in the brain, and thus this contributes to feelings of depression.
Technology-use
In a 2020 study, it was discovered that depression, self-harm, and suicide attempts in U.S. teens significantly increased between 2011 and 2018. It was suggested that an increase in social media and technology use could have played a role in this significant increase.
It was found that heavy users of technology were twice as likely to be depressed or have low well-being compared to light users of technology.
Although technology use is not the cause of most depression, increased time spent on technology may contribute to the sudden increase in depression being diagnosed (Twenge, 2020).
A potential reason why social media may be contributing to depressed feelings is that adolescents and young adults may be making appearance comparisons and judgments to people they see online, which can contribute to increased sensitivity (Hawes et al., 2020), especially in those who are prone to envy and rumination (Zhu et al., 2023).
Although, it could be argued that teens who are experiencing depression anyway may have chosen to use technology more as a way to escape the struggles of daily life, or they may be drawn to technology more if they are isolating themselves from others.
Coping with sadness

It is usually recommended that professional support is sought if one is struggling with feelings of sadness that do not go away.
While therapy can be very helpful, not everyone is always ready to seek help from professionals. Therefore, seeking support from various sources can be an encouraging first step to coping with sadness and depression.
However, for those experiencing the emotion of sadness, there are ways to express sadness healthily to help people get through this emotion. These may also work as preventative methods to stop sadness from turning into depression:
Allowing the sadness
Sadness is a natural emotion that affects all human beings. There is often the thought that sadness should not be felt and that it should be held back/covered up.
However, holding back or not accepting the sadness can be detrimental or even make someone feel worse or even guilty for having these feelings. Sometimes, we have to accept the sadness, letting it wash over us.
Keep in mind that the sadness, along with any other emotion, does eventually pass.
It may be helpful to cry or let out the emotion in a healthy way (e.g., through journalling or talking to a supportive friend) if we need some help with accepting the emotion.
Planning a day to feel sad
If experiencing a lot of sadness, it may be helpful to take a day off to be alone and to reflect on emotions and thoughts. This can help people to move past the sadness into a happier mood.
Think and/or write about what may be causing the sadness
Taking time to understand the context behind the sadness and exploring these feelings can help people feel better.
Take a thoughtful walk
Being in nature with the fresh air and some quiet time, along with some exercise, can help people work through their thoughts and change their perspectives.
Talk to a close friend or family member
Having a support network or even just one person who can be contacted when feeling sad can help people work through their feelings and feel supported.
Being kind to oneself
When feeling sad, it can be useful to do activities that make the individual feel good such as taking a long hot bath, having a nap, or eating their favorite food.
Documenting emotions
Many people find it useful to keep a journal to express their emotions.
This could be used to write down positive things that the individual is grateful for to help them shift their negative perspective to a more positive or realistic one.
It may also be beneficial to write about life goals and the steps that need to be taken to achieve this so that the person has something to focus on and work towards.
Managing depression
Below are some of the ways in which depression can be managed. Keep in mind that this is to be taken as general information and should not be used in place of professional advice. If you or someone you know is struggling with depressed feelings that are interfering with everyday life, it is advisable to seek professional support.
Cognitive behavioral therapy (CBT)
There are many different types of psychotherapy that can help manage the signs of depression. A common type of therapy that has shown to have significant positive effects is CBT.
CBT is a popular therapy and has proved to be even more effective than medications in some instances.
CBT works on tackling the negative thoughts that a person has about themselves and managing these thoughts with something more realistic and helpful.
With the therapist, automatic negative thought patterns can be addressed. Automatic negative thoughts can include negative self-talk that can appear intrusively without necessarily being aware of them. Likewise, in CBT, goals can be set for what the client wants to achieve after completing the sessions.
Activities can be completed during sessions to tackle specific concerns the client may have, as well as ‘homework’ assignments being given, such as completing worksheets or practicing relaxation exercises so that the techniques can be practiced outside the sessions.
Research suggests that CBT can have lasting effects after the sessions are completed and that these effects can often prevent further relapses of depressive signs.
However, it is worth bearing in mind that CBT is not for everyone; some people may relapse after time, and there may be alternative therapies that are just as effective or more so.
Medication
For depression, there are many treatment options available. A doctor may prescribe medicative treatment, which usually will affect the neurotransmitters of the brain. Antidepressants are a common medication for those with depression, and these come in different varieties.
Selective serotonin reuptake inhibitors (SSRIs) are an antidepressant that, as the name suggests, affect the neurotransmitter serotonin. These work by blocking the reuptake (or reabsorption) of serotonin of the presynaptic neuron which released it.
This means there will be more serotonin circulating through the synapse, making it more likely that the chemical will reach the receptors of the next neuron. SSRIs usually take a few weeks to work, but they are widely prescribed for people’s tolerance towards them and their effectiveness in increasing mood and decreasing depressive signs.
However, they come with possible side effects, such as headaches, dry mouth, and nausea.
Serotonin-norepinephrine reuptake inhibitors (SNRIs) are another type of antidepressant that works in the same way as SSRIs in that they block the reuptake of serotonin. Still, they also block the reuptake of the chemical norepinephrine.
This means there will be more of both chemicals circulating in the brain and having a positive effect on mood and depressive signs. In some instances, SNRIs appear to be more effective at treating depression than SSRIs. However, SNRIs tend to produce more side effects and may not be as tolerable as SSRIs.
Monoamine oxidase inhibitors (MAOIs) are an older class of antidepressants that work by blocking the function of the enzymes that break down the neurotransmitters called monoamine oxidase.
If the enzymes are blocked by the MAOIs, there will be more serotonin, dopamine, and norepinephrine circulating around the brain.
These days, MAOIs are not typically prescribed since they have strong and several side effects, as well as dietary restrictions that must be followed if taking this medication.
While there is a lot of support for the use of antidepressants, it is worth bearing in mind that medications work differently for everyone and thus, they may not be the right choice for many people.
Brain stimulation therapies
In cases where other types of therapy do not work, those with severe signs of depression may be advised to try brain stimulation therapies. A type of this is electroconvulsive therapy (ECT), which involves transmitting short electrical impulses into the brain.
When proven unresponsive to other treatments, ECT has produced effective results for those with severe depression.
Most people report improvements after around 4 to 6 treatments, lasting about 10 minutes each time. Some possible side effects of ECT include headaches, nausea, and some memory loss.
Another brain stimulation therapy is transcranial magnetic stimulation (TMS). TMS creates magnetic fields to stimulate neurons in the brain to help improve signs of depression.
With TMS, a large electromagnetic coil is placed on the person’s head, and short pulses are directed into an area of the brain believed to control emotions. Several sessions of TMS of around 40 minutes each are generally required over a period of weeks.
This therapy is not recommended for those with depression with psychosis or those with a high risk of suicide and can have side effects such as muscle contractions in the face and headaches.
Lifestyle
Other ways to treat depression can include exercising, such as aerobic exercise. A systematic review found that aerobic exercise improved the signs of those diagnosed with depression compared with antidepressants or other treatments (Morres et al., 2019).
Likewise, relaxing exercises such as yoga, deep breathing, or meditation could also provide some therapeutic relief for signs of depression.
Finally, eating a healthy diet and getting enough sleep can also contribute to lowering feelings of sadness or depression.
Mindfulness
Mindfulness is the practice of focusing attention on the present moment without distraction. This can be practiced through meditation or even through completing everyday tasks that can help ‘ground’ a person (e.g., while folding laundry, going for a walk, or making a cup of tea).
While using mindfulness to focus on the present moment, we are less likely to be focused on negative thoughts, rumination, or worrying about the future. Thus, mindfulness may help to alleviate mood.
Mindfulness and mindfulness-based stress reduction (MBSR) have been shown to be particularly helpful and cost-effective methods of coping with depression during the COVID-19 pandemic (Behan, 2020).
A questionnaire-based study also suggested that mindfulness practice reduced feelings of depression by reducing levels of worry and rumination (Parmentier et al., 2019).
Can sadness be helpful?
While sadness can be a difficult emotion to experience, it can also serve a useful purpose in our lives. Sadness can be helpful in several ways:
-
Facilitating processing and healing: Sadness can help us process and work through difficult emotions and experiences, allowing us to heal and move forward.
-
Fostering empathy and connection: Sadness can also help us connect with others and build empathy by allowing us to understand and relate to their experiences.
-
Motivating change: Sadness can motivate us to make changes in our lives or take action to address the source of our sadness.
- Identifying values: Sadness can help teach someone about their values by highlighting what is important to them and what they may need to protect or prioritize in their life.
Overall, while sadness can be uncomfortable, it can also serve a purpose and be a valuable emotion in our emotional lives.
Do you need mental health help?
USA
Contact the National Suicide Prevention Lifeline for support and assistance from a trained counselor. If you or a loved one are in immediate danger: https://suicidepreventionlifeline.org/
1-800-273-8255
UK
Contact the Samaritans for support and assistance from a trained counselor: https://www.samaritans.org/; email jo@samaritans.org .
Available 24 hours a day, 365 days a year (this number is FREE to call):
116-123
Rethink Mental Illness: rethink.org
0300 5000 927
Further Reading
References
Behan, C. (2020). The benefits of meditation and mindfulness practices during times of crisis such as COVID-19. Irish journal of psychological medicine, 37(4), 256-258.
Hawes, T., Zimmer-Gembeck, M. J., & Campbell, S. M. (2020). Unique associations of social media use and online appearance preoccupation with depression, anxiety, and appearance rejection sensitivity. Body Image, 33, 66-76.
Khalsa, S. R., McCarthy, K. S., Sharpless, B. A., Barrett, M. S., & Barber, J. P. (2011). Beliefs about the causes of depression and treatment preferences. Journal of clinical psychology, 67(6), 539-549.
Korb, A. (2015). The upward spiral: Using neuroscience to reverse the course of depression, one small change at a time. New Harbinger Publications.
Morres, I. D., Hatzigeorgiadis, A., Stathi, A., Comoutos, N., Arpin‐Cribbie, C., Krommidas, C., & Theodorakis, Y. (2019). Aerobic exercise for adult patients with major depressive disorder in mental health services: A systematic review and meta‐analysis. Depression and anxiety, 36(1), 39-53.
National Alliance on Mental Illness. (n.d.). ECT, TMS and Other Brain Stimulation Therapies. Retrieved 2021, October 15 from: https://www.nami.org/About-Mental-Illness/Treatments/ECT,-TMS-and-Other-Brain-Stimulation-Therapies
Parmentier, F. B., García-Toro, M., García-Campayo, J., Yañez, A. M., Andrés, P., & Gili, M. (2019). Mindfulness and symptoms of depression and anxiety in the general population: The mediating roles of worry, rumination, reappraisal and suppression. Frontiers in psychology, 10, 506.
Truschel, J. (2020, September 25). Depression Definition and DSM-5 Diagnostic Criteria. PSYCOM. https://www.psycom.net/depression-definition-dsm-5-diagnostic-criteria/
Twenge, J. M. (2020). Why increases in adolescent depression may be linked to the technological environment. Current opinion in psychology, 32, 89-94.
World Health Organization. (2021, September 13). Depression. https://www.who.int/news-room/fact-sheets/detail/depression.
Zhu, W., Mou, J., Benyoucef, M., Kim, J., Hong, T., & Chen, S. (2023). Understanding the relationship between social media use and depression: a review of the literature. Online Information Review.

