On This Page:
Mood is a general feeling that can be long-lasting compared to emotions alone which can be fleeting and short-term.
While it is normal to experience periods of different moods, mood disorders are characterized by emotional extremes and difficulties in regulating mood.
Although moods can be temporary, when these moods persist to extremities and cause significant dysfunction, these can cause long-term disturbances.

What Is A Mood Disorder?
Mood disorders are a broad umbrella term used for conditions in which disturbance of mood is the central feature. Common mood disorders include different types of depressive and bipolar disorders.
Mood disorders are found to affect about 20% of the general population at any given time. Specifically, in the US for instance, 17% of the population is thought to struggle with depression over the course of their lifetime, with bipolar disorders affecting 1% of the general population.
Whilst the rate for bipolar disorders is significantly lower, many researchers agree that many instances of manic moods (describing the emotional ‘highs’ of bipolar disorder) often go unnoticed or are deemed unproblematic, meaning that many people may go undiagnosed.
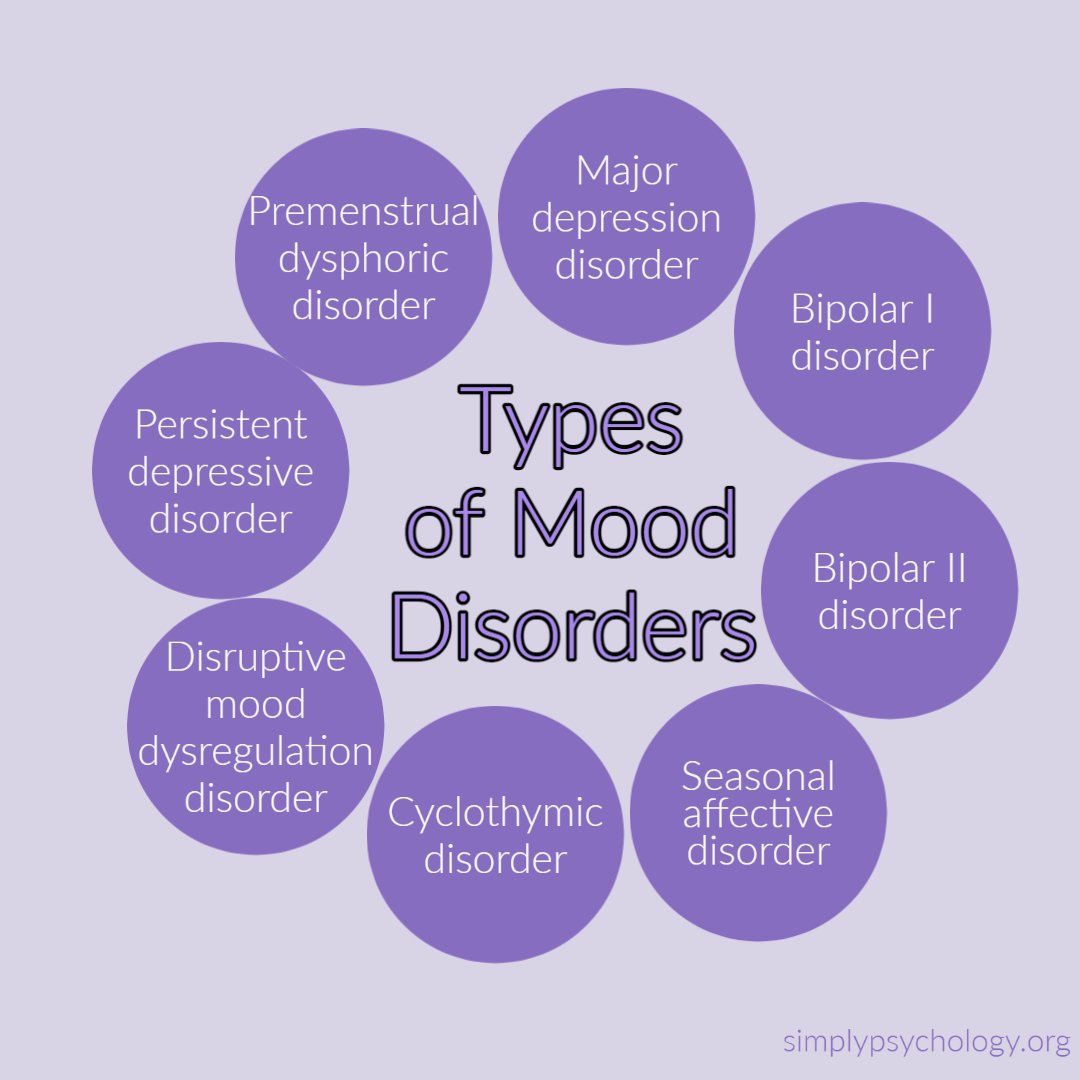
Types of Mood Disorders
Major depressive disorder
Major depressive disorder is characterized by prolonged and persistent periods of extreme sadness.
While it is normal to experience sadness or grief during traumatic life events, if this depression continues even when the events are over, or there is no apparent cause for the sadness, this may classify as clinical or major depression.
This is a very common mental disorder that is accompanied by a variety of physical, cognitive, and emotional symptoms.
Bipolar I disorder
This disorder was formerly known as ‘manic depression,’ characterized by extreme emotional highs and extreme emotional lows that can last for several weeks or longer.
The extreme highs are called mania and involve euphoric and/or irritable moods and increased energy or activity. An individual who experiences mania may present as being over-active and having high levels of energy. They may feel very happy, self-important, have racing thoughts, be unusually talkative, and be easily agitated.
The extreme lows of bipolar I disorder are symptomatic of depression symptoms. They may feel sad, hopeless, lethargic, have difficulty concentrating, feel worthless, and lose interest in everyday activities.
Bipolar I disorder is thought to be the most severe form of bipolar disorder, as manic episodes can cause disruption to everyday life, such as affecting work life and relationships. Someone who is experiencing a manic episode may be more likely to engage in risky behavior, which can have a detrimental impact on their well-being and safety.
Bipolar II disorder
This disorder causes cycles of depression which is similar to those who have bipolar I disorder.
Individuals with bipolar II disorder also experience hypomania, a less severe form of mania.
Hypomanic periods are not as intense or as disruptive as manic episodes, and people are usually able to handle daily tasks despite these episodes.
Seasonal affective disorder (SAD)
SAD is a type of depression that only occurs during certain seasons. Typically, depressed symptoms start in late autumn or early winter for many people, less commonly starting in spring or summer for others.
The symptoms of SAD resemble those of major depression, although SAD differs as the individual will usually start to feel better once the season is over.
Cyclothymic disorder
This disorder is sometimes defined as a milder form of bipolar disorder. It causes emotional highs and lows believed to be less extreme than in those experiencing bipolar I or II disorder.
Individuals with cyclothymic disorder experience continuous irregular mood swings for extended periods. The mood changes can occur suddenly, at any time, with only short periods of baseline mood.
Disruptive mood dysregulation disorder
This is a newer type of depressive disorder that was added to the Diagnostic and Statistical Manual on Mental Disorders (DSM-5).
This is usually diagnosed in children who exhibit persistent irritability and anger with frequent episodes of extreme temper outbursts without any observable cause.
This is often diagnosed when the symptoms are inconsistent with the child’s developmental age.
Persistent depressive disorder
This disorder was previously known as dysthymic disorder, a less severe form of major depression.
This type of depressive disorder is long-term, occurring for at least two years for individuals, and the symptoms of depression occasionally lessen during this time.
Premenstrual dysphoric disorder
This is characterized by mood changes and irritability during the premenstrual stage of a female’s cycle.
They will often experience extreme mood swings, hopelessness, anger, anxiety, or tension. Once the individual begins their menstruation, the symptoms usually cease.
Signs
Below are some of the common symptoms that may be experienced by someone who is experiencing a depressive mood:
-
Loss of interest in activities that were once enjoyed
-
An increase or decrease in appetite
-
Difficulty sleeping or sleeping more than usual
-
Feeling fatigued
-
Being easily upset or crying a lot
-
Feeling isolated
-
Feeling hopeless and worthless
-
Feeling guilty
-
Feeling irritable
-
Physical symptoms such as headaches or stomach aches
-
Low self-esteem
-
Withdrawing from social events, friends, or family
-
Suicidal ideation
-
Difficulty in keeping up with daily tasks and demands of life
Below are some of the common symptoms of manic or hypomanic episodes:
-
Feeling extremely energized or elated
-
Rapid speech
-
Rapid movement
-
Agitation, restlessness, or irritability
-
Risk-taking behaviors
-
Trying to take on many activities at once
-
Racing thoughts
-
Feeling on edge
-
Grandiosity
Often with depressed feelings, this is usually preceded by a number of unhelpful self-statements and thoughts. Usually, there is a pattern to these thoughts, and these are called unhelpful thinking styles.
People tend to use these thinking styles as an automatic habit they may not be aware of.
If someone consistently uses some of the thinking styles, they can often cause themselves a great deal of emotional distress.
-
Mental filter – this includes focusing on only one part of a situation, usually the negative part, ignoring the rest, which may be more positive.
-
Catastrophizing – people may blow something that happens out of proportion. Situations are viewed as more terrible and disastrous than they actually are.
-
Black and white thinking – seeing only one extreme or the other. Someone with this thinking style may only view things as right or wrong, good or bad, with no grey areas in between.
-
Overgeneralization – a person may take one instance in the past or present and impose it on all current or future situations. For instance, they may say, ‘I never…’ or ‘Everyone…’.
-
Jumping to conclusions – people who jump to conclusions tend to assume they know what someone else is thinking (mind reading), and they tend to make predictions about what will happen in the future (predictive thinking).
-
Personalization -with this thinking style, individuals tend to blame themselves for everything that goes wrong or could go wrong. They may take 100% responsibility for the occurrence of external events over which they really would not have control.
-
Shoulding and musting – although not always unhelpful, depending on the situation, saying ‘I should…’ or ‘I must…’ sentences can put unreasonable pressure on the individual.
-
Labeling – this is where the individual makes global statements about themselves and others based on their behavior in specific situations (e.g., ‘I am stupid’, ‘I am worthless’). They may use this label even though there are many more examples that aren’t consistent with that label.
-
Emotional reasoning – this is where people base their view of situations or themselves on the way they are feeling. For example, the only evidence that something bad is going to happen is if they feel anxious.
-
Magnification and minimization – individuals may often magnify the positive attributes of others and minimize their own positive attributes. They may explain away their own positive characteristics or success as though they are not important.
Causes and Risk Factors
While there is not a known direct cause for someone to develop a mood disorder, there are some possible contributing factors that may play a part.
Often, the cause of mood disorders is thought to be a combination of biological, genetic, psychological, and environmental factors.
Genetic factors
Mood disorders have been found to run in families and may have a genetic component. If someone has a close family member, such as a parent, with a mood disorder, this can make it more likely that they will also develop a mood disorder.
However, this could, in part, be an environmental factor because if someone grows up in a household with someone with a mood disorder, it may make it more likely that these traits are picked up or cause systemic issues within the family.
Environmental factors
Likewise, environmental factors such as significant life stress could contribute to someone developing a mood disorder, specifically a depressive disorder.
While a stressful life event is not likely to give someone bipolar disorder, it could trigger a manic or depressive episode in someone with a pre-existing condition.
Comorbidity
Also, if an individual has a history of a previous diagnosis of a mood disorder, it is likely that they are at risk of developing another mood disorder.
Biochemical factors
Brain chemistry could also play a significant role in someone developing mood disorders. The neurotransmitter norepinephrine, which usually increases arousal and focus, appears to be a key chemical.
Norepinephrine is thought to be severely lacking in depressed individuals but significantly high during manic episodes. Also, serotonin, a neurotransmitter responsible for feelings of well-being and happiness, is believed to be significantly low in those with depression.
Medications that affect norepinephrine and serotonin levels in the brain are known to have a positive effect on improving the symptoms of mood disorders, providing evidence that brain chemistry plays a big role in these disorders.
However, for bipolar disorder, the first line of treatment is usually mood stabilizers, as antidepressants can trigger mania.
Biological factors
Another possible factor involved in the development of mood disorders is differences in brain structure in those with mood disorders. There is considerable evidence that the amygdala and medial prefrontal cortical areas are involved in response to emotions and mood disorders (Price & Drevets, 2010).
Closely related to these areas is a network of areas in the central orbital cortex that connects with several sensory-related cortical areas and appears to be critical for assessing objecting and anticipating a reward.
Depressed individuals show abnormalities in this network during functional MRI studies involving reward and emotional processing tasks (Murray et al., 2010).
Also, amygdala volume appears abnormally smaller in individuals with bipolar disorder who are not taking medication but larger in those with bipolar disorder who are receiving mood-stabilizing treatments.
Moreover, depressed individuals tend to show an exaggerated amygdala response when presented with sad words, sad faces, and fearful faces but a blunted response to happy faces (Victor et al., 2010). This suggests the amygdala may play a big role in mood disorders.
Risk factors
Other possible risk factors can include substance abuse and some medications in increasing the likelihood of developing a mood disorder.
Depression is often more diagnosed in women than men, which may imply it is more common in women. However, many believe it may be more diagnosed in women because they tend to seek help more than men.
In a 2020 study, it was found that depression was becoming increasingly common among U.S. adolescents between 2011 and 2018. It was suggested that an increase in social media and technology use could be a risk factor to explain this significant rise in depression.
It was found that heavy users of technology were twice as likely to be depressed or have low well-being compared to light users of technology.
Although technology is not the cause of most depression, an increased time spent on technology may contribute to the sudden increase in depression (Twenge, 2020).
Vicious Cycle of Depression
For those with depressive disorders, the symptoms can change a person’s life, daily routines, and behaviors. Often, it is these changes that make the depression worse and prevent the individual from getting better.
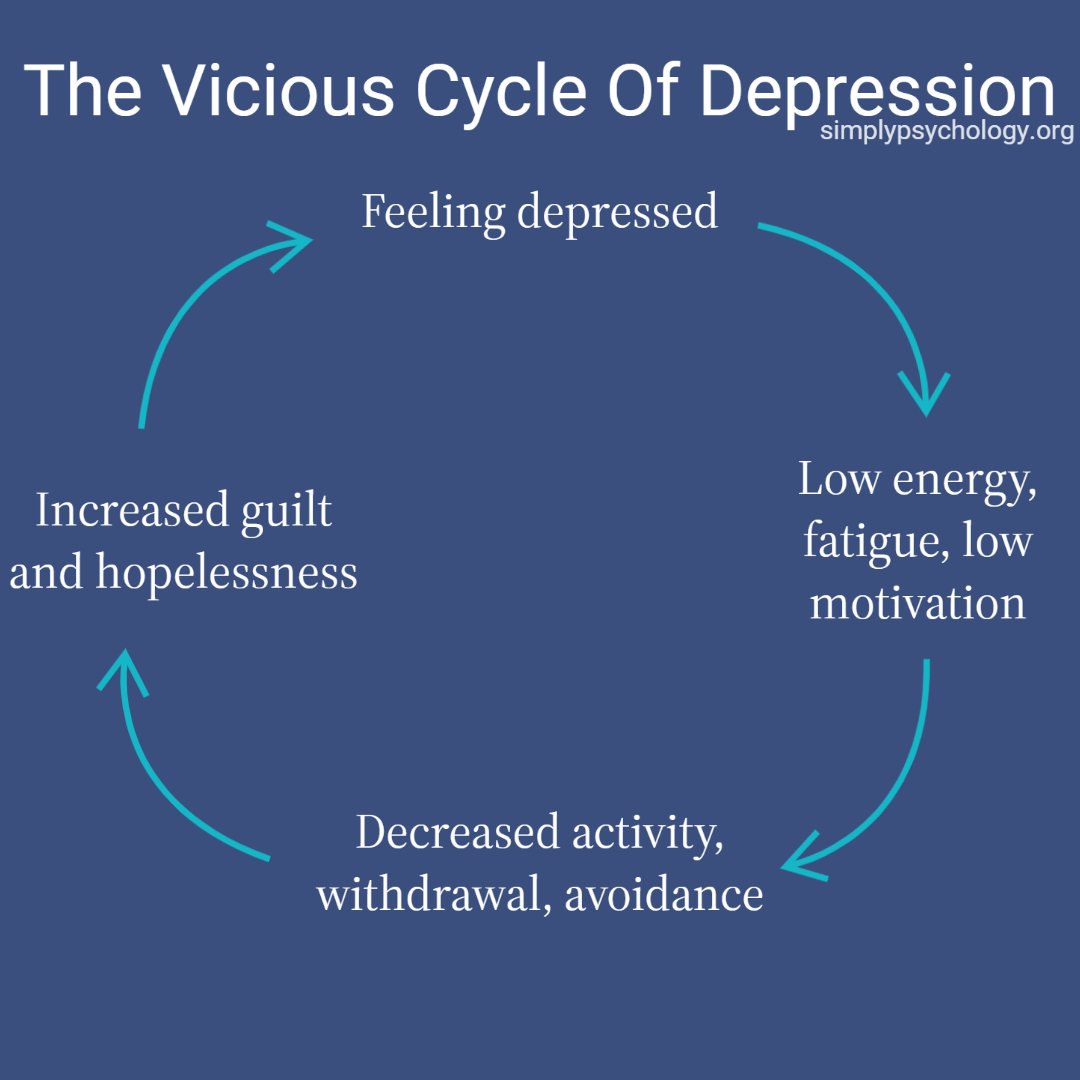
For instance, having a lack of motivation or energy as a result of depression can result in the person disengaging from their usual activities, neglecting their daily tasks, and leaving decision-making to others.
They may find that if they engage less in their usual activities, they may see their friends and family less often. Because of a reduction in activities and not seeing loved ones, they may be locked in a vicious cycle of depression.
Decreased activity and neglecting responsibilities and daily tasks can induce feelings of guilt, hopelessness, and ineffectiveness. This ultimately can lead to stronger depressed feelings, which will mean lower energy, lower engagement in activities, and so on.
Therefore, depression will only get worse if people are stuck in this cycle.
When to Seek Help
It is important to seek help for a possible mood disorder because it is unlikely to go away on its own. The disorder is likely to get worse over time, so seeking help before the disorder becomes more severe can make it easier to treat.
Often, people with bipolar disorder are more likely to seek help when they are experiencing a depressive episode than when they are experiencing mania or hypomania.
Many people may find that they enjoy the extremely elated moods that come with bipolar disorder and thus may be less likely to seek help for this or even recognize that their feelings are a part of the disorder.
If someone suspects that they may have bipolar disorder, it may be useful to keep a mood diary so they can keep track of how they are feeling and see if they notice any unusual patterns in their mood, emotions, and behavior.
If any of the symptoms being experienced seem out of proportion or they have been interfering with life, particularly if having suicidal thoughts, help should be sought as soon as possible.
It is important to talk to a health professional if an individual is feeling like their emotions are interfering with their work, relationships, social activities, or any other areas of their life.
It is also important to seek help if the individual is having trouble with alcohol or drugs, as it is common for many people to rely on substances to cope with their symptoms.
Managing Mood Disorders
If someone is struggling with a mood disorder, there are ways in which to manage the symptoms. Below will discuss some of these management options.
It is important to discuss options with a healthcare provider or mental health professional if the mood disorder is significantly impairing your daily functioning.
Medications
Most medications for mood disorders work on raising serotonin or norepinephrine levels. For depressive disorders, antidepressants are commonly prescribed to increase these neurotransmitter levels.
Often, antidepressants can help change energy levels, improve sleep, and they have proved effective in improving mood. Although different types of antidepressants are found to work equally well, some may be more effective depending on the individual.
If prescribed antidepressants, it is important to take them as prescribed and continue taking them even when starting to feel better. People usually report a significant improvement after taking the medication for 4-6 weeks.
Those who experience mania in bipolar disorder are often prescribed lithium, a mood stabilizer, in the first instance. Mood stabilizers are medications used to help regulate the mood swings that occur with bipolar disorder by reducing abnormal brain activity.
They usually help to protect someone from the extreme highs of a manic episode and the severe lows of a depressive episode. Antipsychotics, previously known as tranquilizers, are generally known to treat psychosis but can also be used to treat bipolar disorder and depression.
They can be especially useful for people with bipolar disorder who experience mania or mixed episodes. They can also sometimes be used to treat depression if symptoms are not controlled with an antidepressant alone.
Psychotherapy
While medications on their own can help alleviate some of the symptoms of mood disorders, health providers often recommend a combination of medication and psychotherapy for more effective treatment.
A popular type of psychotherapy that has proved effective for many is cognitive behavioral therapy (CBT). CBT involves working with a therapist to identify negative thoughts and behaviors, then working on challenging these thoughts and behaviors into more helpful, healthy ones.
This can involve challenging some unhelpful thinking patterns and recognizing when these patterns come up in everyday situations. This therapy has been shown to be especially effective for those with depression.
Brain stimulation therapies
A brain stimulation therapy called electroconvulsive therapy (ECT) has been used to treat severe depression or bipolar disorder when medication or psychotherapy has been unsuccessful.
During this treatment, an electric current is passed through the brain via electrodes attached to the scalp or forehead. The treatment is usually given over 2 or 3 sessions per week, with generally 6 to 12 sessions required for the most effectiveness.
Repetitive transcranial magnetic stimulation (rTMS) is another type of treatment that uses non-invasive magnetic coils to apply short electromagnetic pulses to specific nerve cells in the brain.
The procedure is used to treat major depression for those who do not respond to at least one antidepressant drug and has proven to be useful in improving symptoms.
Light therapy
For seasonal affective disorder, light therapy is common and has proved to be useful for reducing some of the depressive feelings being experienced.
Light therapy involves using light, such as a light box, which supplements natural sunlight with bright artificial light. It is usually recommended to use the light in the mornings for about 20-60 minutes consistently for the most effectiveness.
Lifestyle
Aside from medications and therapeutic treatments for mood disorders, there are some lifestyle changes individuals can make to help reduce their symptoms or as a preventative for mood disorders to begin. Some of these lifestyle changes include:
-
Maintaining a consistent sleep schedule and ensuring getting enough sleep.
-
Keeping a mood diary to note when one is heading towards a manic or depressive episode.
-
Avoiding alcohol and illicit drugs.
-
Eating a healthy and balanced diet.
-
Engaging in regular exercise, especially aerobic exercise.
-
Engaging in yoga, mindfulness, meditation, or other relaxation methods to reduce stress.
-
Maintaining a support network with trusted friends, family, or support groups.
Do you need mental health help?
USA
Contact the National Suicide Prevention Lifeline for support and assistance from a trained counselor. If you or a loved one are in immediate danger: https://suicidepreventionlifeline.org/
1-800-273-8255
UK
Contact the Samaritans for support and assistance from a trained counselor: https://www.samaritans.org/; email jo@samaritans.org .
Available 24 hours a day, 365 days a year (this number is FREE to call):
116-123
Rethink Mental Illness: rethink.org
0300 5000 927
Related Articles
References
Dissociative Disorders. (Jul 05, 2021). 2021 Traumadissociation.com. Retrieved Jul 5, from http://traumadissociation.com/dissociative.
Dissociative Identity Disorder. (Jul 05, 2021). Traumadissociation.com, Retrieved Jul 5, 2021, from h
Murray, E. A., Wise, S. P., & Drevets, W. C. (2011). Localization of dysfunction in major depressive disorder: prefrontal cortex and amygdala. Biological psychiatry, 69(12), e43-e54.
Nathan, P., Rees, C., Lim, L., & Correia, H. (2003). Back from the Bluez. Perth, Western Australia: Centre for Clinical Interventions
Price, J. L., & Drevets, W. C. (2010). Neurocircuitry of mood disorders. Neuropsychopharmacology, 35(1), 192-216.
Price, J. L., & Drevets, W. C. (2012). Neural circuits underlying the pathophysiology of mood disorders. Trends in cognitive sciences, 16(1), 61-71.
Truschel J. (2020, September 29). Bipolar Definition and DSM-5 Diagnostic Criteria. PSYCOM. https://www.psycom.net/bipolar-definition-dsm-5/
Twenge, J. M. (2020). Why increases in adolescent depression may be linked to the technological environment. Current opinion in psychology, 32, 89-94.
Victor, T. A., Furey, M. L., Fromm, S. J., Öhman, A., & Drevets, W. C. (2010). Relationship of emotional processing to masked faces in the amygdala to mood state and treatment in major depressive disorder. Archives of General Psychiatry, 67(11), 1128.


