Hypervigilance is a key feature of post-traumatic stress disorder (PTSD), involving a heightened state of sensory sensitivity and alertness for potential threats.
Individuals with PTSD often experience chronic hypervigilance along with recurrent trauma memories and flashbacks after encountering a severely distressing event.
People with hypervigilance perpetually feel on edge, as though danger could arise at any moment. Their body may be on high alert constantly, making them jumpy, irritable, and unable to relax. This severe form of anxiety can lead to emotional exhaustion and difficulty concentrating.
When hypervigilance occurs due to PTSD, previously non-threatening environments or situations can become loaded with perceived danger, triggering panic and flight-or-fight responses. For example, loud noises, crowded spaces, or media depictions of violence or trauma can all set off acute hypervigilance reactions.

Does Hypervigilance Keep Us Safe?
Sensory stimulation, such as sweaty palms, heart racing, and looking from side to side, is activated to keep us safe during times of danger to prepare us for a freeze, fight, or flight response.
Sometimes, it is activated in response to a perceived threat that is not present; this is also clinically known as hypervigilance.
Hypervigilance is an often fearful, self-protective psychological state of constantly assessing your surroundings. It is critical to help you avoid danger.
Someone who is experiencing hypervigilance elicits amplified sensory sensitivity to their environment, and the nervous system is hyper-aroused to detect possible threats.
This over-stimulation of the nervous system leads to erratic and exaggerated self-defensive behavior in response to a perceived danger that is more than often actually absent.
When experienced for a long period of time, chronic hypervigilance involves a persistent overreaction to a threat that may not exist.
Hypervigilance has many serious implications on quality of life. It can lead to mental exhaustion and difficulty sleeping.
Hypervigilance can produce obsessive patterns due to constantly being hyper-aware of one’s surroundings. Moreover, it can lead to impairments in day-to-day functioning, for example, at work or in social interactions.
Hypervigilance vs. Paranoia
Hypervigilance and paranoia are signs of mental health disorders such as bipolar disorder, anxiety, schizophrenia, and Post Traumatic Stress Disorder (PTSD).
Accordingly, the most prominent sign of PTSD is hypervigilance, while the most prominent sign of schizophrenia is paranoia.
Fear is the underlying emotion of both hypervigilance and paranoia. However, paranoia differs from hypervigilance because it involves irrational thoughts. For example, a paranoid person will have intruding and real thoughts that transcend into delusions. These delusions often have to do with suspicious ideas about other people.
On the other hand, hypervigilance is a state of active threat detection and involves fixated scanning of the environment to watch out for threats.
Individuals who experience hypervigilance have an intense yet disproportionate awareness of their surroundings.
Paranoia is present-focused and involves untrue and specific beliefs about people, while hypervigilance is a future-focused alert state involving fears about impending danger.
Overview of PTSD
Extremely stressful events can leave lasting imprints on an individual’s mental health. Post-traumatic stress disorder (PTSD) is a mental health condition involving frequent psychological disturbances due to a major traumatic event.
A traumatic event is a stressful or threatening experience that is witnessed or experienced. Upon exposure to trauma, PTSD afflicts about 5% to 10% of the population and is higher in women than in men.
PTSD is characterized by the impairment of optimal daily functioning. Some of the signs of PTSD include recurring flashbacks, panic attacks, depression, nightmares, and constant hypervigilance.
Causes of PTSD
PTSD is caused by either witnessing or experiencing a shocking, disturbing, or frightening event. It is commonly seen in post-war veterans, survivors of physical or emotional abuse, serious injuries or accidents, and more.
PTSD can result in chronic hypervigilance due to a constant feeling of uncertainty resulting from traumatic experiences. However, being vigilant is important and, in some cases, useful.
For example, while walking alone at night, chronic sufferers of hypervigilance remain in overdrive even in normal conditions, thus overreacting to triggers that are not really a threat.
This is due to many triggers that send the body into a sustained “fight and flight” mode to protect itself from re-experiencing the trauma.
Common Triggers
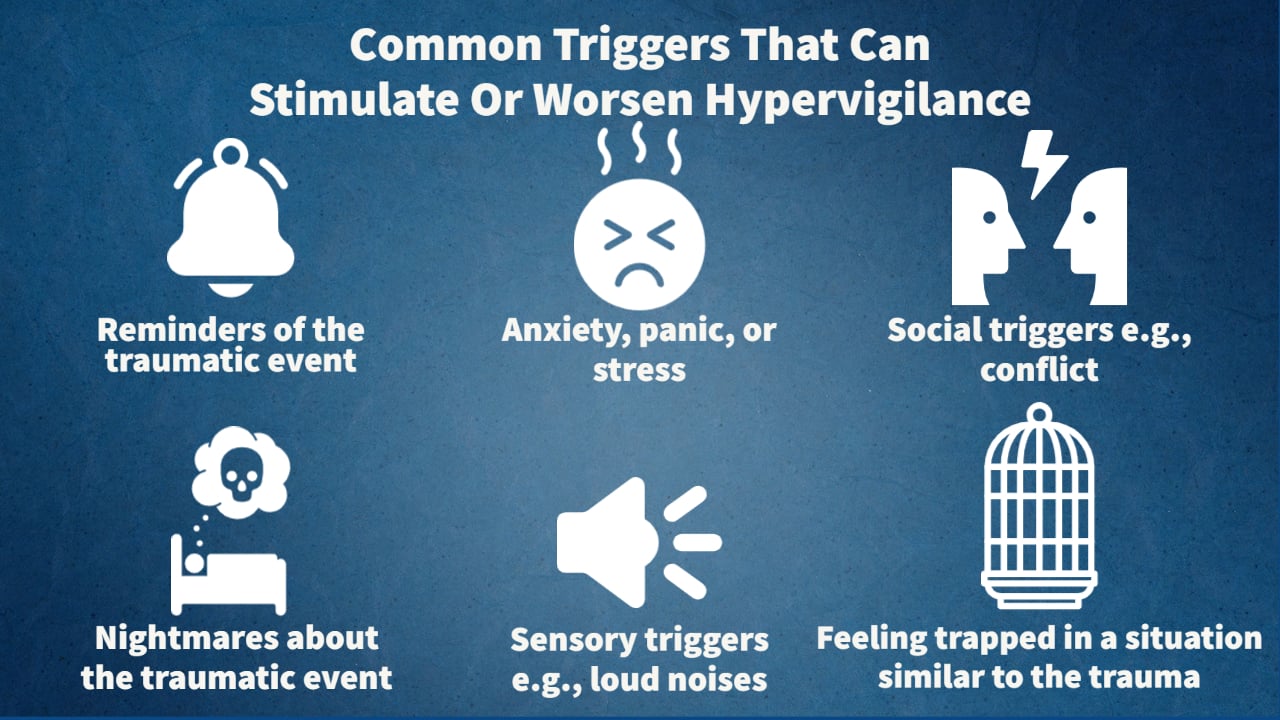
A trigger is a signal that revives past memories, which can then produce psychological and physiological responses.
In the context of PTSD, some of the common triggers that can stimulate or worsen hypervigilance are:
- Reminders of the traumatic event, such as sights, sounds, smells, or sensations associated with the trauma
- Similar environments or situations that resemble the location or context of the traumatic event
- Emotional or physical stressors, such as anxiety, panic attacks, or high levels of stress
- Sleep disturbances or nightmares related to the traumatic event
- Intense emotions, such as fear, anger, or sadness
- Social or interpersonal triggers, such as conflicts, criticism, or rejection
- Substance use or withdrawal from substances as a coping mechanism
- Sensory triggers, such as loud noises, sudden movements, or crowded spaces
- Feeling trapped or powerless in a situation that resembles the traumatic event
- News, media, or conversations about similar traumatic events in the present or past
It’s important to note that triggers can be highly individual and may vary from person to person, and it’s essential to work with a qualified mental health professional to identify and manage triggers for hypervigilance in the context of PTSD.
Signs
Various signs can help detect hypervigilant states. These often fall under three distinct categories.
First, the physiological signs are the body’s physical reactions, while emotional signs are observed through mood and temperament responses.
Finally, behavioral signs are the actions that are elicited as a result of the condition.
It is important to note that the signs of hypervigilant states, especially in PTSD, can vary significantly from person to person. It is possible for someone to experience some, but not all, of the signs listed in this article.
However, it is crucial to emphasize that experiencing one or two signs alone is not sufficient to self-diagnose. A proper diagnosis can only be made by a qualified mental health professional after a comprehensive evaluation.
Physiological Signs
The sympathetic nervous system is activated, causing adrenaline and noradrenaline to be released into the bloodstream in preparation to fight or flight and respond to danger.
This response is evident through the following signs:
-
Dilated pupils
-
Elevated heart rate
-
Increased blood pressure
-
Sweating
-
Rapid breathing
-
Increased sensitivity to pain and emotions
-
Increased energy
-
Easily startled
-
Highly reactive
-
Sleep disturbances
-
Racing thoughts
Emotional Signs
Hypervigilance is an emotionally taxing state. The emotional effects often cause problems in a healthy functioning lifestyle. Some of the most common signs are:
-
Anxiety
-
Flashbacks
-
Restlessness
-
Constant fear or worry
-
Anticipating danger
-
Emotional outbursts
-
Mood swings
-
Anger
In some cases:
-
Emotional withdrawal
-
Detachment
-
Paranoia
Behavioral Signs
Behavioral signs are defense mechanisms that can fall into either avoidance and escape behaviors or confronting and aggressive behaviors.
Some examples of common signs in each category are as follows:
Avoidance & Escape Behaviors
In avoidance, individuals tend to freeze or flee, withdrawing from social settings and isolating themselves.
This can interfere with important pillars of wellness, for example causing relationships to deteriorate.
-
Knee-jerk reactions
-
Substance use and/or abuse
-
Avoiding difficult conversations and confrontation
-
Withdrawn in social settings or new situations
-
Not listening to others
-
Wishful thinking or daydreaming
-
Isolating from friends and family
Confronting and Aggressive Behaviors
People with aggressive and confrontational responses have a proclivity towards fighting or attacking for defense.
This can, at times, lead to trouble with the law.
-
Defensiveness during conversations
-
Overreacting to mundane stimuli
-
Frequently and easily angered
-
Denying any blame
-
Controlling behavior
-
Impulsive aggression
-
Deflecting blame onto others
-
Risk-taking
The Problem with Hypervigilance
Unfortunately, many individuals who experience hypervigilance turn to drugs as a solution to this overstimulation and chronic stress. More specifically, it is estimated that 46.4% of patients with PTSD also have substance use issues (McCauley, 2012).
In addition to substance abuse problems, many people report difficulty falling asleep.
Studies show that in hypervigilance, there is consistent, random, and potentiated activation of the amygdala, which is a brain region associated with emotion regulation and fear.
The insula is another brain region located in the cerebral cortex that is also responsible for regulating emotions as well as processing bodily sensations.
It was found to be active even during sleep in people experiencing hypervigilance. Both the amygdala and insula’s hyperarousal is attributed to troubling factors such as difficulty falling asleep, the feeling of wakefulness during sleep, and an increased perception of pain.
Treatment Options
Fortunately, there are many treatment approaches for hypervigilance.
To understand the signs more deeply, a doctor can help you determine if it is linked to another mental health condition.
Therapy
Therapy involves communicating with a psychotherapist to help you understand and overcome your mental struggles in a collaborative way. Many variations of therapy can be utilized to manage hypervigilance.
A doctor will assess your case to see which approach will work best.
Some of the therapeutic approaches to treatment include Psychoeducation, cognitive processing therapy ( CPT ), exposure therapy, eye movement desensitization and reprocessing (EMDR), and psychoeducation.
Cognitive Behavioral Therapy (CBT)
CBT is a very common type of psychotherapy in which therapists work collaboratively with patients to reframe their thoughts, emotions, and behaviors constructively.
This form of client-centered talk therapy is shown to be highly effective in treating depression, anxiety, addictions, and many more mental health conditions.
Psychoeducation
Psychoeducation is a part of CBT in which a therapist offers knowledge to the patient about their condition, signs, or techniques.
Having awareness about one’s condition has been shown to help in its management.
Exposure Therapy
Many techniques that work for PTSD may be applied to treat hypervigilance, such as exposure therapy, another form of CBT.
Systematic desensitization is a form of exposure therapy in which the individual is exposed to the triggering stimuli and works with a trained professional to address the emotions that arise in a healthy way.
EMDR
Unlike many forms of therapy, Eye movement desensitization and reprocessing (EMDR) does not require the patient to communicate all the aspects of their trauma.
Rather, EDMR therapy incorporates specific eye movements from left to right while clients focus on the traumatic memories. This is thought to initiate the brain’s natural ability to process trauma.
Medication
Medications may help decrease some of the signs of hypervigilance in some cases and are prescribed on a case-by-case basis.
The anxiety that accompanies hypervigilance may be treated with anti-anxiety medication (such as beta-blockers, benzodiazepines, and antidepressants).
Medications may not be the first step to treatment for everyone. It is important to discuss medication with a professional who can determine whether this is right for you as well as outline potential side effects.
Benzodiazepines
Benzodiazepines are GABA agonists. GABA inhibits neuronal activity and acts as the body’s natural tranquilizer by increasing relaxation and inducing drowsiness.
Benzodiazepines are often prescribed to treat anxiety and panic disorder. Therefore, it can help manage the stress associated with hypervigilance.
Some commonly prescribed benzodiazepines include alprazolam, chlordiazepoxide, diazepam, and lorazepam.
Antipsychotics
If hypervigilance is associated with schizophrenia or bipolar disorder, antipsychotics may be prescribed.
Antipsychotics work by blocking the action of dopamine D2, which helps reduce neural activity. This is thought to help reduce psychotic signs and hyperarousal.
Common Antipsychotic medications include quetiapine, aripiprazole, olanzapine, and risperidone.
Antidepressants
Antidepressants are often used to treat depression. However, they can also be used to treat anxiety, pain, and addictions.
The antidepressants widely prescribed for anxiety are selective serotonin reuptake inhibitors (SSRIs).
SSRIs work by inhibiting the reuptake of serotonin, thus increasing the availability of serotonin.
This helps alleviate anxiety and anxiety-related signs such as hypervigilance.
Antidepressants that are frequently prescribed for anxiety include citalopram, escitalopram, fluoxetine, paroxetine, and sertraline.
Beta-blockers
Beta-blockers are commonly prescribed to treat abnormal health rhythms and hypertension but can also help with hypervigilance.
They work by inhibiting the release of adrenaline which is a stress hormone. They allow the heart rate to decrease, which helps lower blood pressure and reduce anxiety.
Some examples of beta-blockers include acebutolol, atenolol, betaxolol, and bisoprolol/hydrochlorothiazide.
Coping Skills
Coping skills are integral to restoring optimal functioning when suffering from hypervigilance and associated mental health concerns.
Prioritizing self-care is the best way to support yourself through this emotionally draining experience and can include daily practices such as:
Mindfulness
Mindfulness exercises can help bring awareness to the emotional state in the present moment. It means being aware of thoughts and emotions without judgment.
A core component of mindfulness exercises is becoming aware of one’s negative thoughts as soon as they surface and instead of following the thought or ruminating on it, it is simply observed and let go.
Breathing
During hypervigilance, the body’s sympathetic nervous system is activated, which is responsible for our fight and flight response and response to potential danger.
Deep breathing is an excellent tool that has been shown to activate the parasympathetic nervous system and stimulate the vagus nerve.
The parasympathetic nervous system is active during relaxation and is often referred to as the rest and digest response. It has the opposite physiological reaction to the sympathetic nervous system.
Exercise
As noted earlier, one of the problems with hypervigilance is that it increases pain sensitivity. To counter this, exercise can be highly effective at mitigating pain.
During exercise, the body releases chemicals known as endorphins. Endorphins bind to opiate receptors and increase positive feelings, similar to morphine. Most importantly, they help reduce pain and stress.
While there is a range of coping skills you can use at home, it can be difficult to address the root cause of hypervigilance on your own.
Therefore, reaching out to an expert could be extremely beneficial and can help you feel safe during recovery.
Hypervigilance is an emotionally draining experience that impacts many areas of your life, from stressful social interactions to difficulty falling asleep.
Overall, seeking treatment can help you identify if it is being caused by another mental health condition along with personal triggers.
Working to find a treatment plan that is best suited to your needs, also known as an individualized treatment approach, is critical in re-establishing mental and physical well-being and ultimately living a happy and healthy life.
Do you need mental health help?
USA
If you or a loved one are struggling with symptoms of PTSD, contact the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline for information on support and treatment facilities in your area.
1-800-662-4357
UK
Contact the Samaritans for support and assistance from a trained counselor: https://www.samaritans.org/; email jo@samaritans.org .
Available 24 hours a day, 365 days a year (this number is FREE to call):
116-123
Rethink Mental Illness: rethink.org
0300 5000 927
References
Campo-Soria, C., Chang, Y., & Weiss, D. S. (2006). Mechanism of action of benzodiazepines on GABAA receptors. British journal of pharmacology, 148(7), 984–990. https://doi.org/10.1038/sj.bjp.0706796
Diagnostic and statistical manual of mental disorders: DSM-5. (5th ed.). (2013). American Psychiatric Association.
Evison, I., Watson, G., Chan, C., & Bridgman, P. (2021). The effects of beta-blockers in patients with stress cardiomyopathy. Internal medicine journal, 51(3), 411–413. https://doi.org/10.1111/imj.15233
Hur, J., Stockbridge, M. D., Fox, A. S., & Shackman, A. J. (2019). Dispositional negativity, cognition, and anxiety disorders: An integrative translational neuroscience framework. Progress in brain research, 247, 375–436. https://doi.org/10.1016/bs.pbr.2019.03.012
Kimble, M., Boxwala, M., Bean, W., Maletsky, K., Halper, J., Spollen, K., & Fleming, K. (2014). The impact of hypervigilance: evidence for a forward feedback loop. Journal of anxiety disorders, 28(2), 241–245. https://doi.org/10.1016/j.janxdis.2013.12.006
McCauley, J. L., Killeen, T., Gros, D. F., Brady, K. T., & Back, S. E. (2012). Posttraumatic Stress Disorder and Co-Occurring Substance Use Disorders: Advances in Assessment and Treatment. Clinical psychology: a publication of the Division of Clinical Psychology of the American Psychological Association, 19(3), 10.1111/cpsp.12006. https://doi.org/10.1111/cpsp.12006
Sprouse-Blum, A. S., Smith, G., Sugai, D., & Parsa, F. D. (2010). Understanding endorphins and their importance in pain management. Hawaii medical journal, 69(3), 70–71.
Strawn, J. R., Geracioti, L., Rajdev, N., Clemenza, K., & Levine, A. (2018). Pharmacotherapy for generalized anxiety disorder in adult and pediatric patients: an evidence-based treatment review. Expert opinion on pharmacotherapy, 19(10), 1057–1070. https://doi.org/10.1080/14656566.2018.1491966
Tseng, & Poppenk, J. (2020). Brain meta-state transitions demarcate thoughts across task contexts exposing the mental noise of trait neuroticism. Nature Communications, 11(1), 3480–3480. https://doi.org/10.1038/s41467-020-17255-9
Van der Kolk B. (2000). Posttraumatic stress disorder and the nature of trauma. Dialogues in clinical neuroscience, 2(1), 7–22. https://doi.org/10.31887/DCNS.2000.2.1/bvdkolk
Weiten, W., McCann, D., & Matheson, D. H. (2022). Psychology: Themes and variations. Cengage. 85-89
Yehuda, R., Hoge, C. W., McFarlane, A. C., Vermetten, E., Lanius, R. A., Nievergelt, C. M., Hobfoll, S. E., Koenen, K. C., Neylan, T. C., & Hyman, S. E. (2015). Post-traumatic stress disorder. Nature reviews. Disease primers, 1, 15057. https://doi.org/10.1038/nrdp.2015.57
You, M., Laborde, S., Zammit, N., Iskra, M., Borges, U., & Dosseville, F. (2021). Single Slow-Paced Breathing Session at Six Cycles per Minute: Investigation of Dose-Response Relationship on Cardiac Vagal Activity. International journal of environmental research and public health, 18(23), 12478. https://doi.org/10.3390/ijerph182312478
Yuan, H., & Silberstein, S. D. (2016). Vagus Nerve and Vagus Nerve Stimulation, a Comprehensive Review: Part I. Headache, 56(1), 71–78. https://doi.org/10.1111/head.12647
Zaccaro, A., Piarulli, A., Laurino, M., Garbella, E., Menicucci, D., Neri, B., & Gemignani, A. (2018). How Breath-Control Can Change Your Life: A Systematic Review on Psycho-Physiological Correlates of Slow Breathing. Frontiers in human neuroscience, 12, 353. https://doi.org/10.3389/fnhum.2018.00353

