Harm OCD is a common subtype of OCD. Individuals suffering from harm OCD will experience aggressive obsessions or unwanted thoughts of violence towards themselves and/or others.
They can spend hours a day preoccupied with fears that they will harm someone close to them or a stranger. Or, they might fear that they have harmed someone in the past and don’t remember it.
“What if I impulsively commit an act of violence against someone?” or “What if I lose control and harm or kill myself?” are thoughts that often arise in harm OCD sufferers. They may also experience urges that suggest it would alleviate their distress if they go through with these violent thoughts.
Individuals feel not only a natural human association with hurting or killing someone but also a concern that they will not be capable of resisting their impulses to act violently and out of control. They view their intrusive and unwanted thoughts as an indication of a desire to act.
Thus, individuals with harm OCD can become obsessed with their need to prove to themselves that they cannot harm others. This fuels their anxiety and drives them to engage in various compulsions, such as hiding objects that might be used to harm others, to eliminate this fear.
In addition, they might engage in a tremendous amount of rumination, becoming obsessed with finding proof that they are not bad people. They can end up searching for confirmation that they are not responsible for harming others or capable of acting out in impulsive and violent ways.
People with harm OCD often become preoccupied with their thoughts. They tend not to be aware that it is natural for all humans to have harmful associations.
Thus, they think enjoying violent content and having aggressive thoughts indicate a character flaw. They believe that because they are having these thoughts, they are more likely to act on them.
They then question their innate characters and assume that having these thoughts makes them bad, violent people.
Examples of Harm OCD Obsessions
Obsessions are unwanted fears and intrusive thoughts. The most common obsessive symptom of harm OCD is the fear of hurting oneself or loved ones.
Harm OCD sufferers either worry that they will harm themselves or someone else by accident (e.g., being afraid to drive because they do not want to cause an accident) or that they will act on an unwanted impulse to harm themselves or another person (e.g., having an impulse to drop their baby and questioning if they secretly actually want to hurt him).
It is common for many people without harm OCD to have brief and momentary thoughts, impulses, or urges to harm oneself or someone else. For example, someone might have a passing thought about stabbing a family member or pushing a stranger in front of a car.
However, they usually do not pay much attention to these thoughts, knowing that they are not going to do that and move on quickly. On the other hand, people with harm OCD will ruminate on these thoughts and are unable to let them go. For example:
- Obsessing over previous mistakes or perceived failures that could have caused harm.
- Worrying about accidentally causing harm while driving, cooking, or handling sharp objects.
- A sudden urge or impulse to harm a friend, loved one, stranger, or animal.
- Fear of losing control and hurting oneself or others accidentally.
- An unwanted impulse to drop a baby.
- An excessive concern with taking too much medication.
- A sudden urge to hurt your spouse or significant other.
- Preoccupation with news or media reports of violent or tragic events.
- Fear of being labeled as violent or aggressive.
Their OCD will assign meaning to the thought, causing people to believe that they genuinely want to commit an act of violence or harm.
This often turns into a preoccupation with preventing harm from happening through compulsions, some of which are described below.
Examples of Harm OCD Compulsions
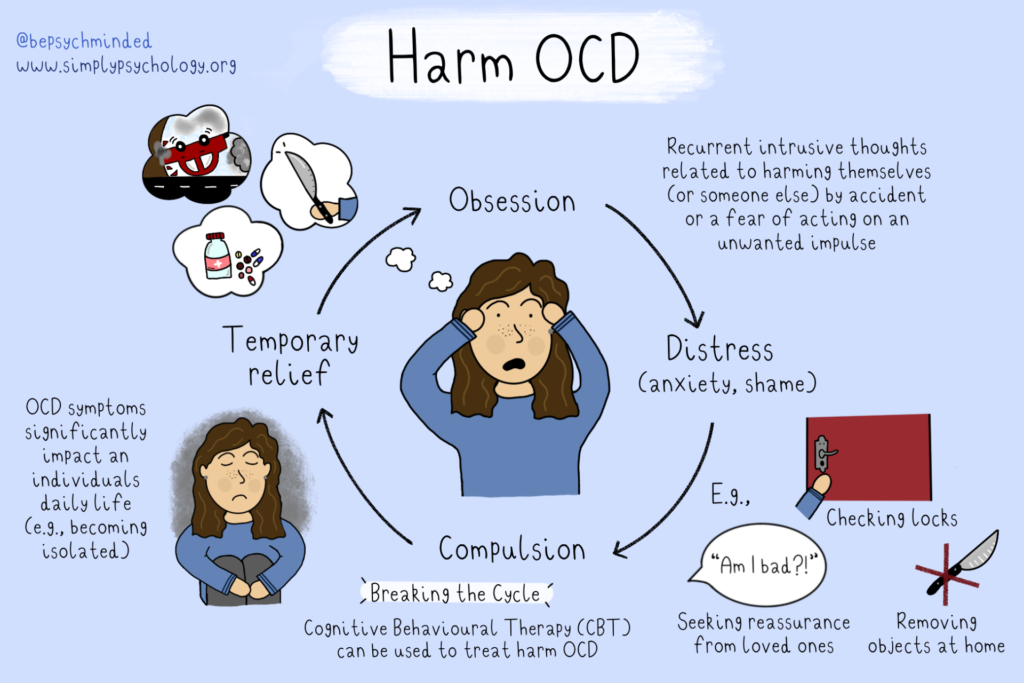
Compulsions are actions and mental rituals performed with the intension to reduce the anxiety. However, this relief is only temporary and actually reinforces the OCD fears and intrusive thoughts (obsessions), making the feeling of anxiety stronger, and thus the urge to perform the compulsion is strengthened by creating an OCD cycle.

Avoidance
People who suffer from harm OCD may avoid situations or activities that trigger their harmful, violent thoughts.
For example, they might avoid window ledges or rooftops because they are afraid they might have an impulse to jump, or a particular restaurant because they experienced an urge to throw their food at the waiter.
They may remove objects from their home, such as knives, chemicals, and medications, to avoid the possibility of obsessive thoughts about harm.
They might also avoid interacting with particular people for fear of experiencing unwanted thoughts, images, or urges toward those individuals.
Reassurance Seeking
An individual may repeatedly ask others for reassurance that they have not caused harm to themselves or others.
A person with harm OCD may seek reassurance from a friend, loved one, or religious leader. They might ask, “Do you think I would actually harm another person or myself?” or “Are you sure I am not a bad person for having these thoughts?”
They also tend to engage in online research to investigate criminals who have harmed others in the past in order to contrast themselves and prove they do not have the same characteristics.
Or, they might research their own violent thoughts to see whether they can become violent acts.
Mental Review
A person who suffers from harm OCD might play out fearful situations in their head to review or practice how they would handle them in real life.
They might also continuously replay past positive experiences in their mind in order to reassure themselves they are not in danger of harming anyone.
For example, they might think that since they were kind to the person they are afraid of hurting, then they do not have to worry about hurting them in the future.
Mental Rituals
Some people with harm OCD will engage in mental, superstitious rituals to counteract the potential harms of an unwanted thought and reassure themselves that they will not act on their violent thoughts, impulses, or urges.
For example, they might count to a lucky number every time a thought comes into their head to counteract these thoughts.
They might also pray, or think of one positive thought for every harmful thought they have to neutralize or replace the negative thoughts.
Checking
An individual may repeatedly check their surroundings or their own body for signs of injury or harm.
For example, they may constantly check the locks on their doors or windows to ensure that nobody can break in and harm them or their loved ones.
Why do Harm OCD Thoughts Happen?
Having unwanted thoughts of violence or committing harm happens for reasons beyond our control and is a normal part of how our brains work.
People with and without OCD have these thoughts. It is not the thoughts themselves that are the problem, but rather the meaning people with OCD attribute to them.
The combination of not wanting to commit a violent act, interpreting violent thoughts as a sign you might do it, and then trying to suppress these harmful thoughts ultimately creates the vicious, obsessive cycle of harm OCD.
According to cognitive-behavioral therapy, people with obsessive-compulsive disorder (OCD) tend to feel like they are responsible for bad things happening to themselves or others.
A person might worry that their obsessive thoughts could lead to something bad happening, which makes them really upset and causes them to do things (like compulsive checking) to try to prevent it.
For instance, someone afraid of leaving the oven on might feel like it’s their job to keep their family safe, so they might check the oven repeatedly to make sure it’s off.
What Happens if Harm OCD is Left Untreated?
Harm OCD can be considered disruptive to one’s daily living if left untreated. The obsessive thoughts and compulsions associated with harm OCD can significantly impact a person’s everyday life and functioning.
Individuals might isolate themselves from friends and family because people with harm OCD tend to avoid certain others that can trigger a fear or obsession.
Sufferers also tend to fear being in public places, which may lead them to not leave their own homes or severely restrict their travel to public places. Additionally, harm OCD thoughts and compulsions can be incredibly time-consuming, draining, and disruptive, taking up hours of a person’s day.
As with all types of OCD, the more a person engages in the obsession-compulsion cycle, the stronger the harm OCD can become.
The pressure and exhaustion associated with this cycle can lead to other severe mental health problems, such as anxiety and depression. The condition can make it challenging to hold a job, maintain a relationship, or simply leave the house.
Similar to other types of OCD, luckily, harm OCD can be managed with appropriate treatment. At least half of the patients who seek treatment for OCD will show symptomatic remission over the long term and experience an increased quality of life and improved functioning.
The best outcomes occur in individuals who are diagnosed early and start an intense treatment program immediately. Depending on the severity of OCD, some people may need longer-term or more intensive treatment.
Harm OCD Treatment
| Treatment | Description | Effectiveness |
|---|---|---|
| Cognitive-Behavioral Therapy (CBT) | A type of psychotherapy that focuses on changing patterns of thinking and behavior. CBT for OCD may involve exposure and response prevention (ERP) techniques, where the individual is gradually exposed to their feared situations and learns to resist compulsions. | CBT has been shown to be highly effective in treating OCD, with many individuals experiencing significant improvement in their symptoms (NICE, 2005). However, despite its widespread use, only around half of patients experience full remission (Farris, et al., 2013). Treatment failure was likely when therapeutic interactions left patients feeling misunderstood, undervalued and/or confused by elements of therapy. |
| Medication | Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), are often prescribed to help manage OCD symptoms. | Medication can be helpful in reducing the severity of symptoms, but may not be effective for everyone. Additionally, some individuals may experience side effects from medication. |
| Mindfulness-Based Interventions | Mindfulness-based interventions, such as mindfulness-based cognitive therapy (MBCT), involve learning to observe and accept thoughts and emotions without judgment. These techniques may help individuals with OCD to learn to relate to their thoughts differently and reduce distress. | Mindfulness-based interventions have shown promise in treating OCD symptoms, but more research is needed to determine their effectiveness for Harm OCD specifically. |
| Acceptance and Commitment Therapy (ACT) | ACT is a type of psychotherapy that focuses on accepting difficult thoughts and emotions while committing to behaviors that align with one’s values. For OCD, this may involve accepting the presence of intrusive thoughts while taking actions that promote safety and well-being. | ACT has shown promise in treating OCD symptoms, but more research is needed to determine its effectiveness. ACT may improve symptoms of OCD to a greater extent than progressive relaxation training. |
| Support Groups | Support groups, such as those offered by the International OCD Foundation, can provide individuals with OCD a safe and supportive environment to share their experiences and learn from others. | Support groups can be a valuable addition to other forms of treatment, but may not be effective as a standalone treatment for OCD. |
Exposure and Response Prevention (EPR)
Like with most types of OCD, the best course of treatment for harm OCD is Exposure and Response Prevention (ERP) therapy. ERP is a type of Cognitive-Behavioral Therapy that is considered the first-line psychotherapy for OCD and has been found effective for 80% of people with OCD.
In ERP, patients are exposed to feared situations or objects meant to set off their compulsions. This therapy is intended to purposely invoke more anxiety in attempts to disrupt the neural circuit between the processing and action parts of the brain.
ERP therapy involves gradually exposing the individual to these feared situations or stimuli while preventing them from engaging in compulsive behaviors or mental acts. Here is an example of a fear hierarchy for Harm OCD:
- Being in the presence of a sharp object such as a knife or scissors
- Holding a weapon or tool that could cause harm
- Being in the presence of someone they care about while holding a weapon or tool that could cause harm
Over time, people learn to resist the urge to perform compulsive rituals and manage their OCD thoughts and actions. By staying in a feared situation without anything terrible happening, they learn that their fearful thoughts are just thoughts and nothing else.
For example, for individuals who have continually experienced fears of hitting someone while driving to the point where this person no longer feels safe driving, the goal of ERP therapy would be to allow this patient to drive again without fear overwhelming them.
In an ERP session, individuals may first start by sitting in the car during a therapy session and allowing uncomfortable thoughts and fears to come up. They will then build up to going for a drive with the therapist until they learn that their feared outcome won’t occur and that they can manage the intrusive thoughts if they arise.
This habituation process of repeatedly invoking anxiety and exposing the brain to a stimulus disrupts the neural circuit between the processing and action parts of the brain.
By staying in a feared situation and leaning into the discomfort and uncertainty, patients learn that they don’t need their compulsions to cope, and that their fearful thoughts have no power over them.
ERP takes time, effort, and practice, but people learn to cope with their thoughts without relying on ritualistic behaviors.
The compulsion to avoid anxiety is a powerful driver of OCD. Still, ERP is one of the most powerful tools available for treating OCD because it directs people with OCD to live with the anxiety and see that nothing bad will happen.
Real-Life Experiences
"I've been dealing with Harm OCD for a few years now. It started with intrusive thoughts about hurting myself, then it moved on to thoughts about hurting others. It was terrifying. I felt like I was losing my mind. But with therapy and medication, I've been able to manage it. It's still a struggle, but I'm not as scared as I used to be. I know now that these thoughts are not a reflection of who I am."
“Harm OCD is a monster. It makes you question your every move, your every thought. It makes you believe you’re capable of the worst possible things. But it’s just that, OCD. It’s not you. It’s taken me a long time to separate myself from my OCD, but it’s been the most important step in my recovery.”
"I've had Harm OCD for about a year now. It's been a roller coaster, to say the least. There are days when I feel like I'm making progress and then there are days when I feel like I'm back at square one. But the one thing I've learned is that it's not about the thoughts, it's about how I react to them. I'm learning to accept them and not give them any power."
Sources
Farris, S. G., McLean, C. P., Van Meter, P. E., Simpson, H. B., & Foa, E. B. (2013). Treatment response, symptom remission, and wellness in obsessive-compulsive disorder. The Journal of clinical psychiatry, 74(7), 21639.
Feliu-Soler, A., Cebolla, A., McCracken, L. M., D’Amico, F., Knapp, M., López-Montoyo, A., … & Luciano, J. V. (2018). Economic impact of third-wave cognitive behavioral therapies: a systematic review and quality assessment of economic evaluations in randomized controlled trials. Behavior therapy, 49(1), 124-147.
Foa, E. B., Sacks, M. B., Tolin, D. F., Prezworski, A., & Amir, N. (2002). Inflated perception of responsibility for harm in OCD patients with and without checking compulsions: a replication and extension. Journal of Anxiety Disorders, 16(4), 443-453.
Hershfield, J. (2018). Overcoming harm OCD: Mindfulness and CBT tools for coping with unwanted violent thoughts. New Harbinger Publications.
Millar, J., Halligan, S. L., Gregory, J., & Salkovskis, P. M. (2020). When Cognitive Behavioural Therapy for Obsessive Compulsive Disorder Fails: Service User Perspectives.
NICE. (2018). Obsessive compulsive disorder and body dysmorphic disorder overview. National Institute for Health and Care Excellence.
Rasmussen, S. A., & Eisen, J. L. (1992). The epidemiology and clinical features of obsessive compulsive disorder. Psychiatric Clinics of North America.
Salkovskis, P. M., Wroe, A. L., Gledhill, A., Morrison, N., Forrester, E., Richards, C., … & Thorpe, S. (2000). Responsibility attitudes and interpretations are characteristic of obsessive compulsive disorder. Behaviour research and therapy, 38(4), 347-372.
Skapinakis, P., Caldwell, D. M., Hollingworth, W., Bryden, P., Fineberg, N. A., Salkovskis, P., … & Lewis, G. (2016). Pharmacological and psychotherapeutic interventions for management of obsessive-compulsive disorder in adults: a systematic review and network meta-analysis. The Lancet Psychiatry, 3(8), 730-739.
FAQs
Does having harm OCD mean I am a dangerous person or will act on my thoughts?
No, having Harm OCD does not mean you are a dangerous person or that you will act on your intrusive thoughts.
People with Harm OCD experience unwanted, distressing thoughts about causing harm to themselves or others, but these thoughts are not aligned with their true feelings, intentions, or desires.
In fact, individuals with Harm OCD are often deeply disturbed and distressed by their thoughts, which is why they engage in compulsions or safety behaviors to neutralize the anxiety and prevent the imagined harm from occurring.
This is a key distinction between having intrusive thoughts due to Harm OCD and having actual intentions to cause harm.


